DOI: 10.20986/resed.2019.3696/2018
ORIGINAL
Optimization of postoperative pain management based on a new technological tool. Pain map
D. Samper Bernal1, P. Barroso Castaño2, G. Roca Amatria3, M. Pérez Hinarejos4, M. M. Monerris Tabasco5, L. García Eroles6 y R. López Alarcón7
1Jefe de Sección Clínica del Dolor, 2Enfermera Clínica de la Unidad de Dolor Agudo, 3Adjunta de la Clínica del Dolor, 4Enfermera Supervisora y 5Adjunta de la Clínica del Dolor. Servicio de Anestesiología, Reanimación y Terapéutica del dolor. Hospital Universitario Germans Trias i Pujol. Badalona. 6Gerente de Sistemas de Información. Servicio Catalán de la Salud. 7Dirección de Organización y Sistemas de Información. Gerencia Territorial Metropolitana Norte. Instituto Catalán de la Salud. España
Received: 04-07-2018
Accepted: 20-01-2019
Correspondence: Daniel Samper Bernal
dsamperb@gmail.com
ABSTRACT
Introduction: In 2005, the Ministry of Health, Social Services and Equality (MSSSI) promoted the Patient Safety Strategy of the National Health System (SNS), in collaboration with the Autonomous Communities, which integrated the contributions of health professionals and patients through their organizations.
One of the objectives of safe practices was the need for prevention and control of pain in adults and children, including management of the same in quality standards.
At the Germans Trias and Pujol University Hospital (HUGTIP) in 2016, the development of the indicators that were intended to be evaluated for better detection and therapeutic efficiency of acute in-hospital pain in any area ended with the design and creation of what we call as “Pain map”.
The objective was to design a tool that, through the clinical pain variable, could improve the visualization of pain and extract statistical data from the defined indicators for optimal pain management in a university hospital of the third level.
Material and method: Descriptive analysis of the tool we call "Pain map" at the Germans Trias and Pujol University Hospital during 2016. The population was all patients admitted to hospital units where the pain registry was made through the GacelaCare® computerized medical record.
The main variable was the recording of pain intensity using the Visual Analogue Scale (VAS) or Numeric Verbal Scale (NVA) by nursing shift considering pain as the 5th constant. The tool creation procedure was carried out with the collaboration of the hospital information systems department together with members of the Pain Unit for the elaboration of the so-called pain map.
Results: The "Pain map" is based on the previous action required by nursing which is the recording of the intensity of pain using the Visual Analogue Scale (VAS) or Numerical Verbal Scale (NVA) in turn considering pain as the 5th constant.
The map allows to visualize on the screen the registers of the pain intensity of all hospitalized patients simultaneously and in real time.
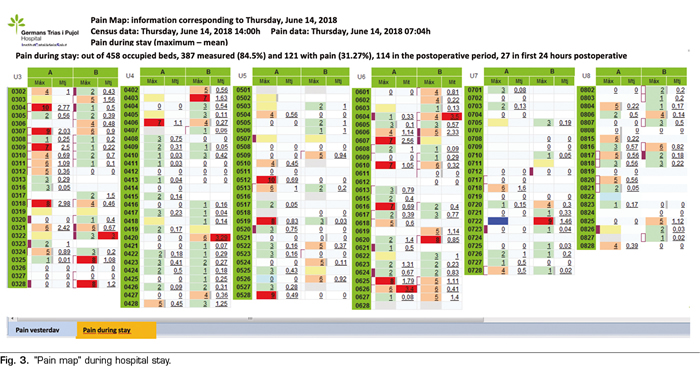
The "Pain map" identifies with different colors as a traffic light of pain. In green color, the EVN values are between 0-3 (mild pain), orange EVN between 4 and 6 (moderate pain) and red color between 7 and 10 (intense pain). Likewise, it indicates with a purple band those patients operated on the previous day, facilitating pain control during the first 24 postoperative hours.
The statistical exploitation of computerized pain registers allows obtaining results of the quality indicators related to pain management defined by our hospital.
Discussion: The "Pain map" is an innovative tool that allows the development of low-cost Acute Pain Units to be guaranteed with efficiency.
Key words: Pain, pain management, integrated and advanced information management systems, indicators of quality in health care, postoperative pain.
RESUMEN
Introducción: En el año 2005 el Ministerio de Sanidad, Servicios Sociales e Igualdad (MSSSI) impulsó y promovió la Estrategia de Seguridad del Paciente del Sistema Nacional de Salud (SNS), en colaboración con las comunidades autónomas, que integraba las aportaciones de los profesionales sanitarios y de los pacientes a través de sus organizaciones.
Uno de los objetivos de las prácticas seguras era la necesidad de prevención y control del dolor en el adulto y en el niño, incluyéndose la gestión de este en los estándares de calidad.
En el Hospital Universitario Germans Trias i Pujol (HUGTIP), en el año 2016 se inició la elaboración de los indicadores que se querían evaluar para una mejor detección y eficiencia terapéutica del dolor agudo intrahospitalario de cualquier área y que finalizó con el diseño y creación de lo que denominamos “Mapa del dolor”.
El objetivo fue diseñar una herramienta que, a través de la variable clínica dolor, permitiera mejorar la visualización de esta y extraer los datos estadísticos de los indicadores definidos para una óptima gestión del dolor dentro de un hospital universitario de tercer nivel.
Material y método: Análisis descriptivo de la herramienta que denominamos “Mapa del dolor” en el Hospital Universitario Germans Trias i Pujol (HUGTiP) durante el año 2016. Se incluyeron todos los pacientes ingresados en los que el registro de dolor se realizó a través de la historia clínica informatizada GacelaCare®.
Considerando el dolor como 5.ª constante, la variable principal fue el registro de la intensidad del dolor mediante la escala visual analógica (EVA) o escala verbal numérica (EVN) en cada turno de enfermería. El procedimiento de creación de la herramienta para la elaboración del denominado “Mapa del dolor” se realizó con la colaboración del Departamento de Sistemas de Información del HUGTiP, junto con miembros de la Unidad del Dolor.
Resultados: El “Mapa del dolor” se fundamenta en el registro de la intensidad del dolor mediante la escala visual analógica (EVA) o escala verbal numérica (EVN) por turno de enfermería, acción previa imprescindible por parte de enfermería. Permite visualizar en la pantalla los registros de la intensidad del dolor de todos los pacientes hospitalizados de manera simultánea y en tiempo real.
El “Mapa del dolor” identifica los registros con distintos colores a modo de semáforo del dolor, en color verde marca los valores de EVN entre 1-3 (dolor leve), en color naranja EVN entre 4-6 (dolor moderado) y en color rojo EVN entre 7-10 (dolor intenso); asimismo señala con una franja de color morado aquellos pacientes operados el día anterior, facilitando el control del dolor durante las primeras 24 horas postoperatorias.
La explotación estadística de los registros informatizados de dolor permite obtener resultados de los indicadores relacionados con su gestión, previamente definidos por nuestro hospital.
Discusión: El “Mapa del dolor” es una herramienta innovadora que permite desarrollar con garantías la eficiencia de las unidades de dolor agudo de bajo coste.
Palabras clave: Dolor, manejo del dolor, sistemas integrados y avanzados de gestión de la información, indicadores de calidad de la atención de salud, dolor postoperatorio.
INTRODUCTION
The Ministry of Health, Social Services and Equality (MSSSI in Spanish), in collaboration with the governments of the autonomous regions, launched and promoted in 2005 the Patient Safety Strategy of the National Health System (SNS in Spanish), integrating the contributions of healthcare professionals and patients through their organizations (1,2).
The objectives of this strategy were based on improving the safety culture, the management of health risk, the training of professionals, the implementation of safe practices, and the involvement of patients and citizens.
The healthcare centers should develop effective systems to ensure, through the Clinical Directorate, a safe care and to learn lessons from their own practice and that of others (3).
One of the objectives of safe practices would be the need to prevent and control pain in adults and children (4-6), including the management of pain within the standards of “Achieving Improved Measurement” of the Canadian Council on Health Services Accreditation (7).
At the Germans Trias i Pujol University Hospital, from 1990 to date, strategies and resources have been gradually implemented to improve pain control, ranging from the use of patient-controlled analgesia pumps (PCA) in the 90s until the establishment of the Pain Committee in 2009, with a broad representation of members of medical and surgical services and nursing teams.
This Committee has been and it is the engine that, in less than a decade, has consolidated the efficiency in the control of pain by creating the figure of the pain nurse in each unit of hospitalization and critical care, the protocolization of all the acute pain of all surgical and medical services and the systematic analysis of the prevalence of in-hospital pain. This Committee has also established the continuous training of all nursing staff through a monographic course conducted biannually (of which 14 editions have been conducted to date), being the incorporation of the acute pain clinical nurse specialist from 2015 the last action conducted by this committee.
Furthermore, information and communication technologies (ICT), initially aimed at the management of hospital resources, have now been opened to monitor and control clinical variables. Therefore, in 2016, using their resources, the elaboration of indicators of acute inpatient pain began.
The objective was to design a tool that, through the clinical variable pain, could improve the visualization of this variable, extracting also the statistical data of the defined indicators for an optimal pain management.
MATERIAL AND METHOD
Descriptive analysis of the tool called “Pain map” in the Germans Trias i Pujol University Hospital in 2016.
The studied population consisted of all the admitted patients in whom pain was recorded using the GacelaCare® computerized medical record.
The main variable was the recording of pain intensity using the Visual Analogue Scale (VAS) or Verbal Numerical Scale (VNS); considering pain as the 5th constant, this information was recorded during each nursing shift.
The procedure for the creation of the tool was performed with the collaboration of the Department of Information Systems and members of the Pain Committee. The objectives were to optimize the visualization of pain intensity records, and thus to define the indicators for a better detection and therapeutic efficiency of acute in-hospital pain. This tool was integrated into the “Business Objects” (BO) system, which obtains data from GacelaCare®.
The implementation of the new tool was performed simultaneously in 10 units of adult hospitalization and 1 unit of pediatric hospitalization at the end of 2016. In 2017, the Renal Transplant Unit and the new hospitalization unit for patients with psychiatric disorders were incorporated, thus completing the record in all the hospitalization units of our center.
The daily visualization of this tool is conducted by the acute pain clinical nurse, identifying those patients with high records of pain, in order to assess the causes and to optimize the analgesic regimen under the supervision of the physician assigned to the unit.
Records with severe pain are evaluated together with the patient’s nurse, and with the pain nurse and the supervisor of each of the hospitalization units.
RESULTS
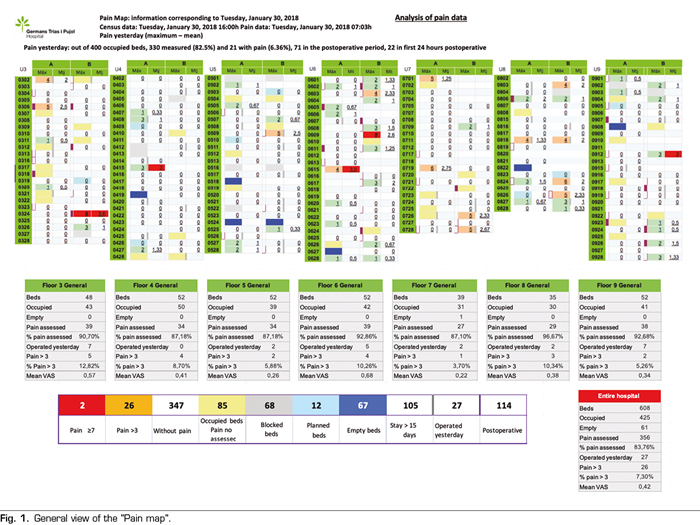
The "Pain map" allows to visualize records of pain intensity of all inpatients simultaneously and in real time (Figure 1).
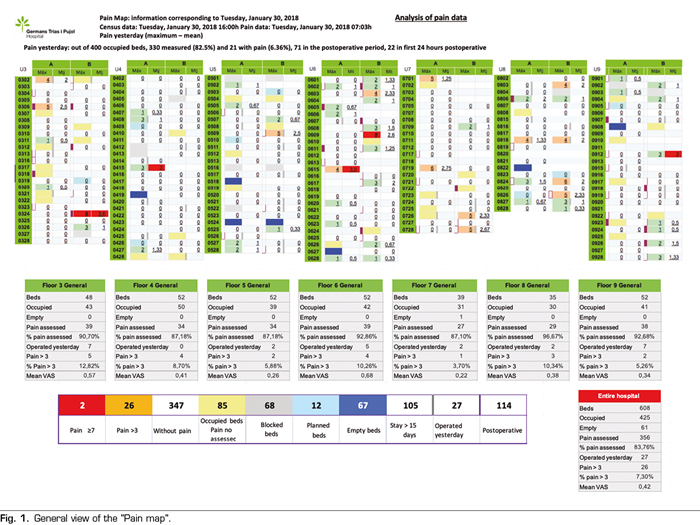
The “Pain map”, designed in a very visual way, identifies the intensity of the pain with different colors similarly to a traffic light. It shows the VNS values using the following colors: 1-3 (mild pain) in green, 4-6 (moderate pain) in orange, and 7-10 (intense pain) in red. In addition, the pain map points out with a purple band those patients operated on the previous day, facilitating pain control during the first 24 hours after surgery (Figure 2).
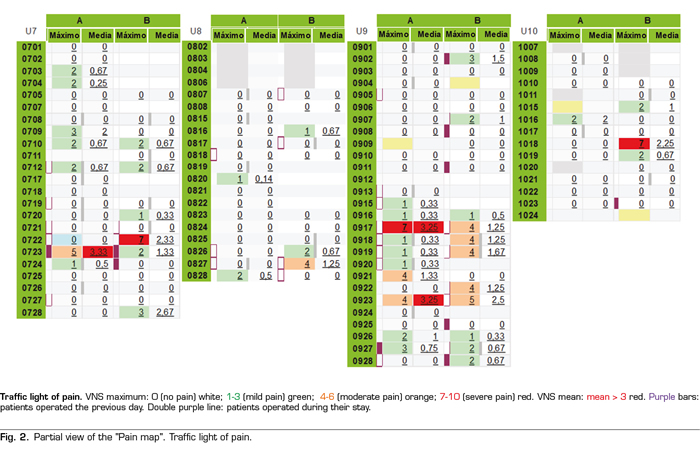
Two visualization schemes are available: one scheme provides information that allows detecting all those patients who have or have had pain in the last 24 hours, and the other scheme provides information regarding the entire hospital stay (Figure 3).
This information is the spearhead that starts, from the Acute Pain Unit, all those actions aimed at alleviating, as much as possible, pain in these patients.
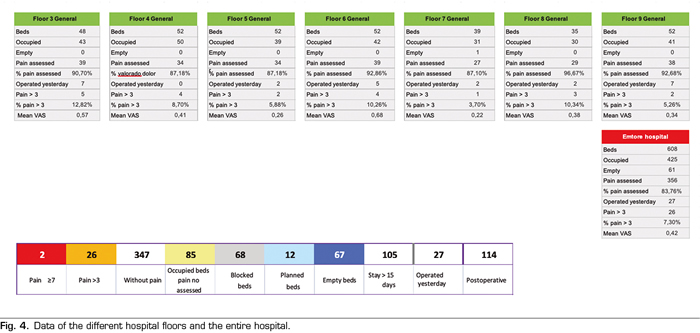
The lower part of the pain map shows the general information per hospitalization floor and the whole hospital with description of empty beds, occupied beds, percentages of patients included in the pain record per nursing shift, number of patients operated in the last 24 hours and percentage of patients with VNS pain> 3 and mean VNS (Figure 4).
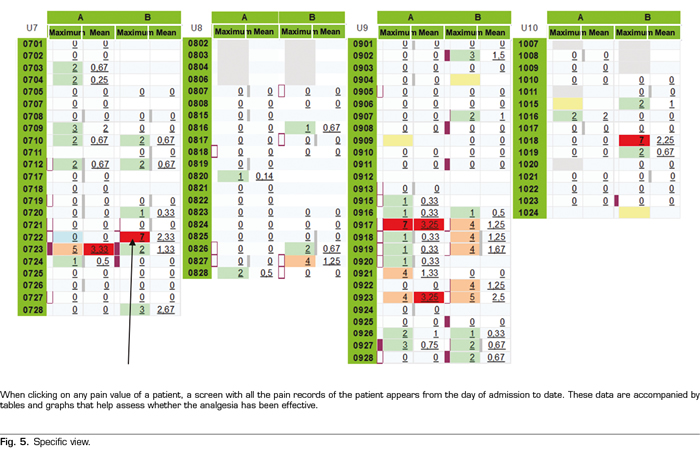
The display screen of each patient is accessible by pressing any value of VNS in the pain map. Subsequently, a screen with all the pain records will appear from the moment the patient was admitted until the last record registered. This information is accompanied by tables and graphs that help to assess whether the analgesia used was effective (Figures 5 and 6).

In addition, the “Pain map” identifies whether a patient has had a peak of pain (VNS ≥ 7) and whether an effective analgesic rescue has been administered (one and two hours after this pain peak), an action that demonstrates if the intervention was quick and effective during an intense pain (Figure 6).
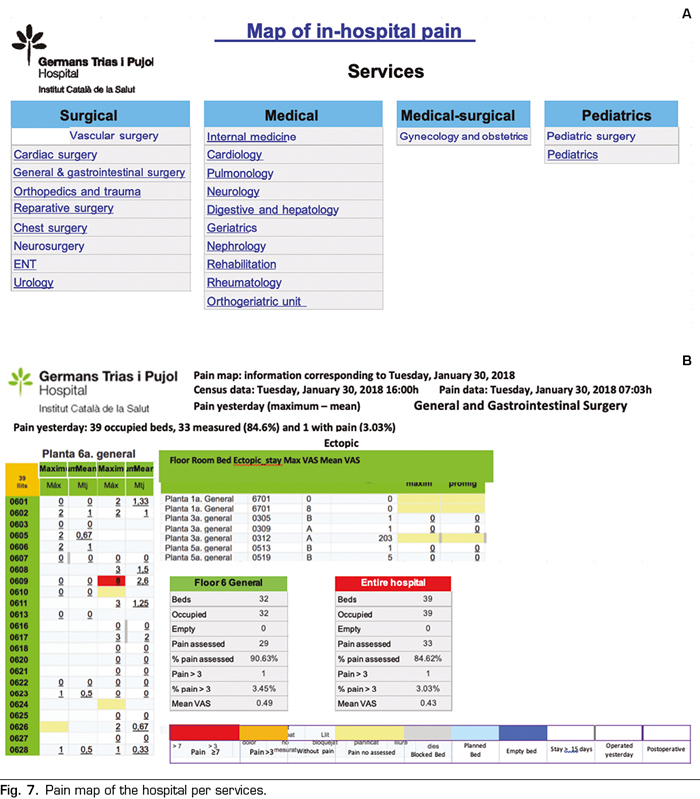
By using filters, the tool allows data mining separately for each medical or surgical service and in each hospitalization floor, facilitating the assessment of pain management in each of these environments (Figure 7).
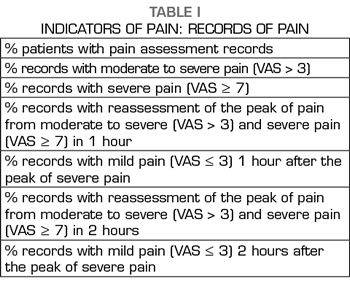
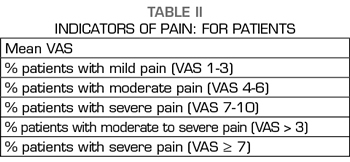
In the absence of the acute pain indicators proposed by scientific societies, those indicators that we consider essential to assess the efficiency of in-hospital pain were defined. Special emphasis has been placed on the effectiveness of the actions undertaken against an intense pain with the aim of identifying problems and implementing measures of improvement.
Among the selected indicators, we considered of great interest those evaluating the VNS record, at least, on each nursing shift. In order to achieve the best outcomes on these indicators, the nursing training on the importance of the correct recording of pain and the reassessment of pain after an episode of intense pain (VAS ≥ 7) was intensified.
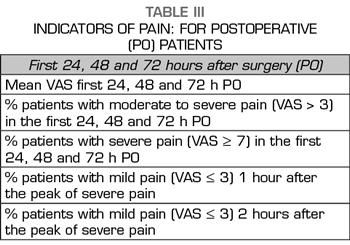
Considering that the most intense post-surgical pain does not occur only during the first 24 hours, but also between 48 and 72 hours, which is when the postoperative patient intensifies mobilization, respiratory physiotherapy, rehabilitation, etc., indicators were established throughout this period. The results of these indicators of acute postoperative pain have allowed us to reassess the protocols of analgesic regimen, especially in those fast-track surgeries where analgesic optimization at early discharge is critical.
The statistical mining of these data makes it possible to obtain comparative tables of these quality indicators, which allows the monthly elaboration of reports that are sent to all those responsible for the services and hospitalization units (Tables I, II and III). This action allows a transversal management of hospital pain control.
DISCUSSION
Information and Communication Technologies (ICT) in healthcare are key tools to improve the quality of healthcare and the health of citizens, facilitate the work of professionals and make healthcare centers more efficient (8).
The “Pain map” allows to visualize in real time the VNS values of all inpatients (9), being a fundamental management tool for the Acute Pain Unit.
Specific training in the field of pain, especially in Nursing but also to physicians, is an essential action for pain control. The designation of the clinical pain nurse, in conjunction with the development of ICT, allows the optimization of pain control, guaranteeing the efficacy, safety and quality of care. The potential of this measurement tool has marked many of the following strategies: to use correctly the different pain assessment scales, to improve the degree of compliance with the assessment and record in the medical record, to correct the incorrect practices through the involvement and training of the healthcare professionals, to apply the different therapeutic measures (pharmacological and non-pharmacological), to improve the assessment of the effectiveness of the applied treatment, to optimize the action against an intense pain, to inform patients about pain management, and finally to minimize the risk of errors in the administration of analgesia.
We believe that achieving excellence in the control of acute pain will be a reality when pain in movement is controlled (cough, bowel movements, deep breathing, joint movements, ambulation, etc.). However, we must be realistic and this will not be achieved unless we are able to control pain at rest first.
The indicators of pain should therefore contemplate both pain at rest and in movement.
This control tool is intended to be the initial step to respond to all inpatients with pain from rest to full functionality.
In conclusion, all these strategies have as a final goal the achievement of larger efficiency in pain measurement and treatment in our hospital.
The “Pain map” is an innovative inexpensive tool facilitating the management of Acute Pain Units.
BIBLIOGRAPHY