DOI: 10.20986/resed.2019.3707/2018
ORIGINAL
Role of depressive symptomatology, catastrophism and expectation in the efficacy of interventional treatment in chronic low back pain
M. A. Ramírez Huaranga1, I. V. de la Rocha Vedia1, A. E. Plasencia Ezaine1, C. A. Jaramillo Tascón1, J. H. Calle Ochoa1 y A. López López2
1Unidad de Tratamiento del Dolor Crónico, Hospital General Universitario de Ciudad Real, Ciudad Real, España. 2Profesora Titular, Universidad Rey Juan Carlos, Madrid, España
ABSTRACT
Objective: To determine the predictive value of psychological variables (depressive symptomatology, catastrophism and expectation) in the success of the therapeutic sacroiliac joint injection for the treatment of chronic low back pain.
Methodology: An observational, descriptive cross-sectional pilot study (May-June 2017) in new patients with chronic lumbar pain of sacroiliac origin without psychological/psychiatric previous disorder who had never undergone any type of infiltration. An initial clinical assessment was made, a structured questionnaire was applied to determine the presence of the variables expectation, catastrophism and depressive symptomatology. An ultrasound-guided sacroiliac infiltration was scheduled and a new clinical comparative assessment was performed after 4 weeks.
Results: 28 patients were obtained (75% women) with an average age of 60+/-11.8 years. A baseline VAS was 7.64+/-1.42 and basaline EuroQol of 0.451+/-0.202. After 4 weeks of the procedure, the VAS was 6.32+/-1.66 and the EuroQol was 0.594+/-0.242. Although all the variables showed a relevant role in the clinical response, the catastrophism was the greatest associated with poor clinical improvement (p=0.001).
Conclusions: The detection and early treatment of vulnerability variables such as depressive symptomatology, catastrophism and the level of expectation are determining factor to obtaining better therapeutic outcomes in patients with chronic pain.
Key words: Expectation, catastrophism, depression, chronic back pain, interventional treatment.
RESUMEN
Objetivo: Determinar el valor predictivo de las variables sintomatología depresiva, nivel de catastrofismo y expectativa en el éxito de la infiltración terapéutica de la articulación sacroilíaca para el tratamiento del dolor lumbar crónico.
Material y métodos: Estudio piloto observacional, descriptivo de tipo transversal (mayo-junio de 2017) en pacientes nuevos con dolor lumbar crónico de origen sacroilíaco sin trastorno psicológico/psiquiátrico previo y a los que nunca se les había realizado ningún tipo de infiltración. Se hizo una valoración clínica inicial y se aplicó un cuestionario estructurado para determinar la presencia de las variables expectativa, catastrofismo y sintomatología depresiva. Se programó para la realización de una infiltración sacroilíaca ecoguiada y posteriormente se realizó una nueva valoración clínica comparativa a las 4 semanas.
Resultados: Participaron 28 pacientes (75 % mujeres), con una media de edad de 60 ± 11,8 años. La puntuación basal en la escala visual analógica (EVA) fue de 7,64 ± 1,42 y la puntuación basal en el EuroQol fue de 0,451 ± 0,202. A las 4 semanas del procedimiento la EVA fue de 6,32 ± 1,66 y el EuroQol de 0,594 ± 0,242. Si bien todas las variables estudiadas mostraron un papel relevante en la respuesta clínica, la variable catastrofismo fue la que presentó mayor asociación con una escasa mejoría clínica (p = 0,001).
Conclusiones: La detección y tratamiento precoces de variables de vulnerabilidad como la sintomatología depresiva, el grado de catastrofismo y el nivel de expectativa son determinantes para la obtención de mejores resultados terapéuticos en los pacientes con dolor crónico.
Palabras clave: Expectativa, catastrofismo, depresión, dolor lumbar crónico, intervencionismo.
Received: 10-08-2018
Accepted: 20-04-2019
Correspondence: Marco Aurelio Ramírez Huaranga
hurauma@hotmail.com
INTRODUCTION
Pain is a complex and multidimensional phenomenon in which the individual not only has a perceptive experience but also an affective one, which is conditioned by multiple biological, sociocultural and mainly psychic interactive components, so that cognitive, emotional and personality variables seem to explain the individual differences in perception and pain tolerance. Likewise, other factors such as the coping strategies, beliefs of uncontrollability of pain and catastrophic thoughts are associated with greater inability, maladjustment and worse response to treatment (1-3).
Since 1975, several studies mention the need to perform screening tests that determine which psychological characteristics can predict the success of pain therapies, given that certain psychological factors (personality disorders, anxiety, depression, poor adherence to treatment, coping strategies and negative expectations) are associated with poorer functional outcomes among patients with chronic pain (4-6). Therefore, current clinical guidelines recommend a routine psychological assessment in this group of patients (7).
In a systematic review of predictive factors of the success of back surgery, it was observed that psychological factors (depression, anxiety, somatization and hypochondriasis states and negative coping) were determinant in 70% of the studies for a negative clinical outcome (8). Regarding the type of coping, previous studies reflect positive differences in response to treatment in patients with active coping strategies (9,10).
The aim of our study was to determine the predictive value of the depressive symptomatology, catastrophism level and expectation variables in the success of the therapeutic infiltration of the sacroiliac joint for the treatment of chronic low back pain.
MATERIAL AND METHODS
Observational, descriptive and cross-sectional study conducted between May and June 2017 at the Chronic Pain Treatment Unit of the General University Hospital of Ciudad Real.
The varied structural origin of low back pain means that the possibilities of interventional treatment are different from one person to another. Therefore, it was decided to conduct the study only in those who met the following criteria:
– Inclusion criteria:
• New patients who attended for the first time the Chronic Pain Treatment Unit (to avoid that previous experiences could condition the expectations and outcomes).
• Patients with chronic low back pain (more than 6 months).
• Pain located in the sacroiliac joint that reproduces under pressure and provocative maneuvers.
– Exclusion criteria:
• Presence of prior psychological/psychiatric disorder.
Given the previous statistics of our Unit, new patients with chronic low back pain of sacroiliac origin attended each month are usually approximately 12 to 16. Being a small population (without taking into account those who did not want to participate in the study or who could not be included), it was decided to work with the entire population that met the inclusion/exclusion criteria.
Clinical assessment and psychological tests were performed on the day of the first visit. Subsequently, ultrasound-guided infiltration of the sacroiliac joint with local anesthetic (0.25% levobupivacaine) and depot triamcinolone was performed by the same doctor. Finally, a new clinical assessment was performed 4 weeks after the procedure.
The variables studied were:
– Sociodemographic variables: age (years) and sex (male/female).
– Clinical variables: chronicity of pain (months); VAS 1-10 (0 = no pain, 1-4 = mild pain, 5-7 = moderate pain, 8-10 = severe pain) and EuroQol; total daily dose and type of pharmacological treatment (scheduled and rescue).
– Independent variables:
• Expectation of pain change after the interventional procedure: low (0 and +1), medium (+2 and +3) and high (+4 and +5).
• Catastrophism: pain catastrophizing scale of Sullivan (11) (adaptation to Spanish); presence of catastrophism > 0 = 13 points (12,13).
• Depressive symptomatology: CES-D scale consisting of 20 items (14) (adaptation to Spanish (15)); presence of clinically depressive symptoms ≥ 16 points.
– Dependent variables:
• VAS: The decrease in the degree of pain to one of the lower grades will be considered as improvement.
• EuroQol-5D: the increase in the numerical value compared to the previous value will be considered as improvement.
• Decrease in analgesic medication: need of less than 50% of the usual dose of rescue analgesia and/or decrease of 50% of the scheduled analgesic dose.
In the data analysis, the odds ratio (OR) and the comparison of means for the association between the presence of negative psychological factors and clinical improvement after interventional treatments were determined. All the analyses were performed with a 95% confidence interval (CI) and the statistical software SPSS 18.0 was used. The study protocol was approved by the Ethics and Research Committee of the General University Hospital of Ciudad Real on April 25, 2017 and was recorded in the 04/2017 minute.
RESULTS
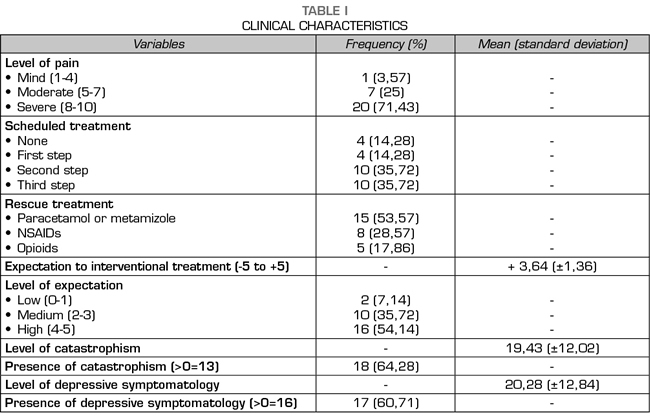
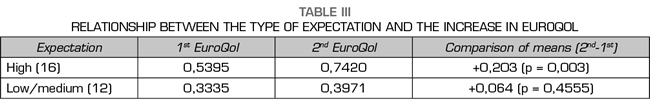
During the study period, 31 patients were selected meeting the inclusion/exclusion criteria. A total of 28 out of 31 patients agreed to participate: 21 (75%) were females, with an average age of 60 (±11.8) years, a time course of 20.2 (±7.8) months , a VAS score at the beginning of the study of 7.64 ± 1.42 and a baseline EuroQol score of 0.451 ± 0.202. The remaining clinical characteristics are described in Table I.
Four weeks after the procedure, the average VAS was 6.32 ± 1.66. A reduction of more than 50% in the scheduled analgesia in 4 patients (16.66%) and a reduction of more than 50% in the rescue analgesia in 19 patients (67.85 %) and a EuroQol of 0.594 ± 0.242 were obtained.
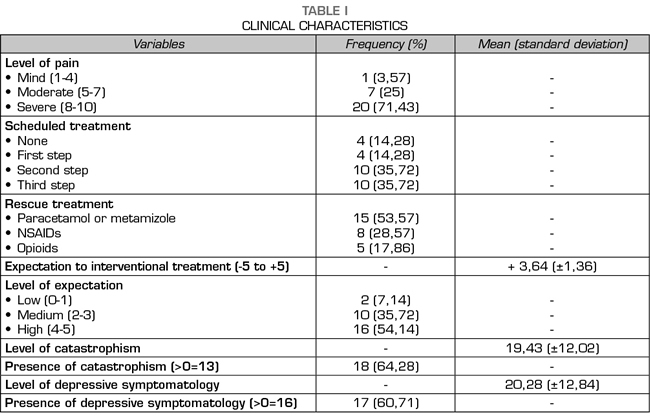
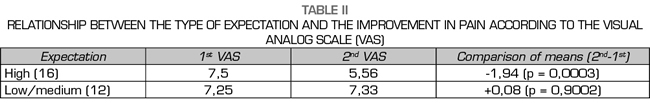
The patients with high expectation had a significant decrease in the VAS of -1.94 (p = 0.0003) and a rise of the EuroQol of +0.203 (p = 0.003), while in the medium/low expectation group this decrease in VAS was nonsignificant (p = 0.9) nor was the increase in EuroQol (p = 0.455) (Tables II and III). A high expectation was a predictive factor for improvement for both the decrease in VAS (OR 13, 95% CI 2.12-79.59, p = 0.0061) and the reduction in rescue analgesia (OR 89.57, 95% CI 4.16-1927.37, p = 0.0001).
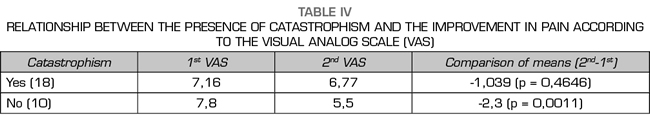
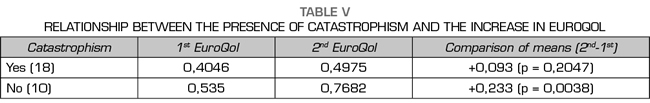
Patients with catastrophism (score ≥ 13 points) did not show a significant decrease in the mean of the VAS (p = 0.464) or a rise in the EuroQol (p = 0.204), whereas in the group of patients without catastrophism the decrease in the VAS (p = 0.001) and the increase of the EuroQol (p=0.003) were significant (Tables IV and V). The absence of catastrophism was a predictive factor for improvement for the three variables studied: decrease in VAS (OR 32.2, 95% CI 1.63-635.5, p = 0.0016),
reduction in scheduled analgesia (OR 15.95, 95% CI 1.29-174.39, p = 0.0277) and reduction in rescue analgesia (OR 21, 95% CI 1.07-411.86, p = 0.009).
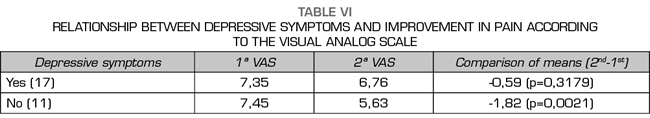
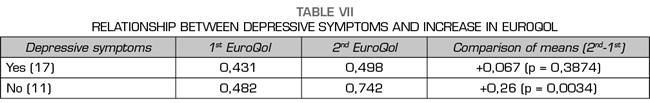
Patients with depressive symptomatology (score ≥ 16 points) did not present a significant decrease in the mean VAS (p = 0.317) or a rise in the EuroQol (p = 0.387), whereas in the group of patients without depressive symptomatology the decrease in VAS (p = 0.002) and the increase in EuroQol (p = 0.003) were significant (Tables VI and VII). In the analysis of association, the absence of depressive symptomatology was a significant predictor of improvement only for the reduction in scheduled analgesia (OR 51.86, 95% CI 2.3-1771.12, p = 0.001).
DISCUSSION
The identification of psychological factors predictive of response to treatment in patients with chronic low back pain is of utmost importance. As they are potentially modifiable, their assessment is recommended at the beginning of the therapeutic approach of the patient with pain (16-18). In our series, the prevalence of low level and medium level of expectation to interventional treatment was 7.14% and 35.72%, respectively; whereas 64.28% of patients presented catastrophism and 60.71% of patients presented depressive symptoms.
The expectation to treatment is a variable that can be influenced by several factors. The interpersonal communication between the patient and the physician and the detailed information on the diagnosis, plan and objective of the treatment are decisive to generate real and positive expectations in patients (19,20). A Canadian study conducted in 2272 patients with chronic noncancer pain showed that a high level of expectation (pain relief of 90-100%) in patients undergoing multidisciplinary treatment (educational, psychological, pharmacological and physical therapy) resulted in a significant decrease in pain level (p < 0.005) (21). Regarding low back pain, a Norwegian study conducted in 246 patients found that a negative expectation is more likely to keep the sick leave for more than 3 months (OR 4.2, 95% CI 1.7-10) after an episode of acute/subacute low back pain (22). A Swiss study with 100 patients operated on in the spine showed that the presence of a high level of positive expectation was the factor most related to a sustained decrease in pain level (VAS) and an improvement in functional capacity (Roland-Morris questionnaire) (p = 0.001) (23). A Swedish study, performed in 59 patients undergoing lumbar discectomy, found that the clinical outcomes obtained at 2 years of follow-up were significantly better in those patients who had a high level of positive expectation of returning to work for both pain intensity (p = 0.03) and functionality (p < 0.001) (24). In our study, we found that patients showing a high expectation of clinical improvement after performing an interventional procedure for the treatment of pain had 13 times greater chance (95% CI 2.12-79.59; p = 0.0061) to present a decrease in the level of previous pain and clinical improvement quantified by VAS (p = 0.0003) and EuroQol (p = 0.003). Indirectly, this improvement was observed through the decrease in the consumption of rescue analgesics (p = 0.0001).
The studies available on catastrophism and pain are more abundant. Regarding low back pain, a Dutch study conducted in 1845 patients with musculoskeletal pain found that a high degree of baseline catastrophism was an excellent predictor of persistence of high pain levels and functional limitation in patients with low back pain at 6 months of follow-up (OR 1.7-3.0) (25). Regarding lumbar interventionism, an observational study of a Korean cohort consisting of 138 patients operated on for stenosis of the lumbar canal showed a positive correlation between high levels of catastrophism and persistence of high pain levels (VAS) and functional limitation (Oswestry index) 3 years after the intervention (Pearson’s correlation coefficient 0.658-0.845, p < 0.001) (26). However, a study performed in Spain in a total of 1422 patients with low back pain failed to show that the degree of baseline catastrophism could predict the clinical course (OR 0.87, 95% CI 0.58-1.31, p = 0.509) (27). In our study, we found that patients with catastrophism presented an increased risk of poor clinical improvement (p = 0.0016), which translated into a nonsignificant decrease in VAS (p = 0.464) or improvement in the EuroQol (p = 0.204), as well as in the decrease in the consumption of both scheduled (p = 0.0277) and rescue (p = 0.009) analgesics after performing an interventional procedure for the treatment of pain.
Chronic low back pain and depression are two of the most common problems faced by healthcare professionals, mainly due to the prevalence of a depressive state that can vary between 16.4% and 73.3% and because of their association with a decrease in the effectiveness of pain treatments (28). With regard to the treatment of spinal pathology, a cross-sectional study conducted in 537 patients found that patients with depressive symptoms presented significantly worse developmental outcomes (p < 0.001) after the intervention: Oswestry back pain disability scale (36 -42 vs. 16), presence of pain (81-88% vs. 40%) and continuous use of analgesic medication (93% vs. 71%) (29). In our study, we found that patients with depressive symptoms did not present an increased risk of poor clinical improvement
(p = 0.115), but it was indirectly reflected in a nonsignificant decrease in VAS (p = 0.317) and in a non-improvement in the EuroQol (p = 0.387) after performing an interventional procedure for the treatment of pain.
Therefore, we can conclude that there is a clear association between the presence of psychological factors of vulnerability (absence of high expectation, catastrophism and depressive symptomatology) and a poor clinical response after performing an interventional procedure for pain relief, showing the presence of catastrophism the greatest association.
LIMITATIONS
Due to the period of inclusion of cases and the selectivity of the patients included in this pilot study, the population size with whom we worked was small. However, the results obtained are consistent with those described in other studies, which encourages the continuation of studies in this area and under a similar methodology to achieve a larger sample that provides greater statistical power.
ACKNOWLEDGMENTS
A special thanks to the entire team of the Chronic Pain Treatment Unit of the General University Hospital of Ciudad Real for their dedication and great teamwork.
REFERENCES