DOI: 10.20986/resed.2020.3840/2020
REVIEW
TRANSITIONAL PAIN CLINIC
CLÍNICA DE DOLOR TRANSICIONAL
M. Bolívar1-4
M. Toro2-4
M. E. Seijas2
A. Bolívar1
M. Bolívar (Jr)1
1Hospital de Clínicas Caracas. Caracas, Venezuela
2Instituto Médico La Floresta. Caracas, Venezuela
3Grupo Médico Santa Paula. Caracas, Venezuela
4Curso de Perfeccionamiento Profesional en Medicina del Dolor. Universidad Central de Venezuela. Caracas, Venezuela
ABSTRACT
Persistent postoperative pain is pain that develops after a surgical procedure, which the patient did not present before surgery. It is becoming more and more frequent and a prevalence ranging between 10 % and 50 % of adult patients undergoing major surgery is reported. It should be considered an important public health problem not only because of the anguish and disability it produces, but it may have contributed to the opioid epidemic in the 1980s, and part of the tools used for its treatment may have contributed to this crisis in the United States, by promoting the long-term use of opioids in patients with non-cancer pain.
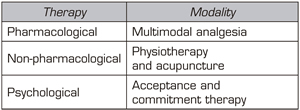
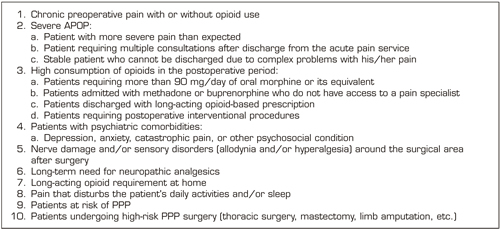
In order to reduce the severity of postoperative acute pain, a fundamental risk factor involved in the origin of PPP, multidisciplinary approaches are required, aimed at preventing and treating the different risk factors that anticipate this disease. This is how the Transitional Pain Service or Transitional Pain Clinic appears in 2014. It is a novel program that aims to effectively control of acute postoperative acute pain, facilitate opioid weaning, reduce the development of chronic pain disability, and help decrease deaths related to opioid over prescription. This model of care was created to effectively manage patients' perioperative pain, maintain function, reduce opioid use, and monitor the efficacy of these interventions. It focuses on persistent postoperative pain in three stages: 1) pre-operative, 2) post-operative in the hospital setting, 3) post-operative in the outpatient setting up to 6 months after surgery. This program offers services focused on: 1) Introduction and optimization of multimodal analgesia, to improve pain management and facilitate weaning from opioids; 2) Non-pharmacological interventions including physical therapy and acupuncture; and 3) Psychological interventions by a trained pain psychology team, around an acceptance and commitment therapy model.
The new situation we are experiencing with COVID-19 demands innovations in medical care, as non-urgent medical care is reduced or abolished and it is time to look for different options from conventional ones for patient follow-up, it is the time of Telehealth. For now, it is necessary to leverage Video Tele Heath and Transitional Pain Service to continue monitoring our patients.
Key words: Pain, chronic pain, anaesthesia, perioperative pain treatment, acute pain services, transitional pain services
RESUMEN
El dolor posoperatorio persistente es un dolor que se desarrolla posterior a un procedimiento quirúrgico que el paciente no lo presentaba antes de la cirugía. Es cada vez más frecuente y se reporta una prevalencia que oscila entre el 10 y el 50 % de los pacientes adultos sometidos a cirugía mayor. Debe ser considerado un problema de salud pública importante, no solo por la angustia y discapacidad que produce, sino porque pudo haber contribuido con la epidemia de los opioides en la década de los años 80, ya que parte de las herramientas usadas para su tratamiento pudo haber contribuido a esa crisis en los Estados Unidos, al promoverse el uso de los opioides a largo plazo en pacientes con dolor de tipo no oncológico.
Para lograr disminuir la severidad del dolor agudo posoperatorio, factor de riesgo fundamental involucrado en el origen del dolor posoperatorio persistente, se requiere de enfoques multidisciplinarios dirigidos a prevenir y tratar los diferentes factores de riesgo que anticipan esta enfermedad. Es así como aparece en el año 2014 el Servicio de Dolor Transicional o Clínica de Dolor Transicional. Es un programa novedoso que tiene como objetivo controlar eficazmente el dolor agudo posoperatorio, facilitar el destete de opioides, reducir el desarrollo de la discapacidad por dolor crónico y ayudar a disminuir las muertes relacionadas con la prescripción excesiva de opioides. Este modelo de atención se creó para controlar eficazmente el dolor perioperatorio de los pacientes, mantener la función, reducir el consumo de opioides y controlar la eficacia de estas intervenciones. Se enfoca en el DPP en tres etapas: 1) preoperatorio, 2) posoperatorio en el ámbito hospitalario, 3) posoperatorio en el ámbito ambulatorio hasta 6 meses después de la cirugía.
Los servicios que ofrece este programa se enfocan en: 1) introducción y optimización de la analgesia multimodal para mejorar el manejo del dolor y facilitar el destete de los opioides; 2) intervenciones no farmacológicas, que incluyen la fisioterapia y la acupuntura; y 3) intervenciones psicológicas realizadas por un equipo de psicología del dolor capacitado en torno a un modelo de Terapia de Aceptación y Compromiso.
La nueva situación que vivimos con la COVID-19 demanda de innovaciones en la atención médica al disminuirse o abolirse atenciones médicas no urgentes, y es el momento de buscar opciones diferentes a las convencionales para el seguimiento de los pacientes; es el tiempo de la telesalud. Se impone por ahora apalancarnos en vídeo Tele Salud y los servicios de dolor transicional para seguir controlando nuestros pacientes.
Palabras clave: Dolor, dolor crónico, anestesia, tratamiento del dolor perioperatorio, servicios de dolor agudo, servicios de dolor transicional
Received: August 14, 2020
Accepted: November 24-2020
Correspondence: Marcos Bolívar Bolívar
mjbolivar2005@gmail.com
INTRODUCTION
In the last 20 years, important advances have been made in the management of acute postoperative pain (APOP). However, the incidence of persistent postoperative pain (PPP), also called chronic postoperative pain, has not significantly decreased (1,2). Surgery produces postoperative pain that must be relieved as soon as possible and as effectively as possible to reduce suffering, promote the healing and rehabilitation process, and prevent complications. APOP, as a manifestation of acute pain, is a more complex phenomenon than was thought years ago, and its potential for chronification is high. For this reason, its therapeutic approach cannot be simplistic, it must be approached at different levels of the nociception process. Additionally, we know that the pain caused by surgery occurs at a known time, it is anticipated. For these reasons, we should identify risk factors and decrease peripheral and central sensitization of the nervous system responsible for primary and secondary hyperalgesia, reducing the possibility of chronic pain. Despite all this, the clinical management of postoperative pain is far from being successful, resulting in a high incidence of severe postoperative pain, many of these patients will develope chronic pain.
Although neural tissue damage and inflammation occur, the pathophysiology of postoperative pain is unique and the consequences are specific. However, the treatment strategies commonly used are not yet based on these findings, in addition to the lack of analgesics and techniques with limited adverse effects and/or with benefits directed at specific aspects of postoperative pain (3,4,5).
From a pathophysiological point of view, APOP has two components: inflammatory and neuropathic.
Inflammatory pain occurs in response to the release of local inflammatory mediators after a painful stimulus. These substances, called by some inflammatory soup, will lower the excitation threshold of peripheral nociceptors, which is called peripheral sensitization, which is responsible for primary hyperalgesia (pain in the surgical scar). A neuronal depolarization is generated that will be transmitted through the peripheral pathways to the dorsal horn of the spinal cord, magnifying the pain signal and calling it central sensitization, which is responsible for secondary hyperalgesia (pain around the surgical scar). These changes are usually reversible, of known onset and end generally related to tissue repair, in addition to responding to non-steroidal anti-inflammatory drugs, acetaminophen (paracetamol) and opioids.
The neuropathic component develops after an injury in the nerves or sensory transmitting systems of the spinal cord and brain. There is a loss of sensitivity with paradoxical hypersensitivity that results in the appearance of sensory phenomena such as: loss of sensations of touch, temperature, pressure, spontaneous pain, dysesthesias, allodynia, hyperalgesia and hyperpathia. This pain, once established, will not respond to the aforementioned analgesics for inflammatory pain and it is present in postoperative pain syndromes (5).
The eleventh revision of the International Classification of Diseases defines PPP as pain that develops or increases in intensity after a surgical procedure, in the area of surgery, that persists beyond the healing process (that is, at least three months) and that is not explained by another cause, such as infection, malignancy or a pre-existing pain condition (6). The prevalence of this chronic pain remains high, being reported between 10% and 50% of adults undergoing major surgery (7,8). It can appear with any surgery, however it has a high prevalence in thoracic and breast surgery, inguinal hernia, low back spine, hip, knee and trauma surgeries and burns (9). The PPP is an important public health problem, not only because of the distress and disability it produces, but it could have contributed to the opioid epidemic in the 1980s, because part of the tools used for its treatment may have contributed to that crisis in the United States (10). The long-term use of opioids in patients with non-cancer pain was promoted at that time (11).
To reduce the transition from APOP to PPP, multidisciplinary approaches are required to prevent and treat the different risk factors that anticipate this disease (3,4,5,12). This is how transitional pain services (TPS) appeared in 2014 (13,14), and later the transitional pain clinics (TPC) (15).
In countries such as Finland, an outpatient clinic of the acute pain service has been used to follow up patients at risk of PPP, suggesting the results of patients evaluated an average of five risk factors for the development of the disease. This conception implies the early, preoperative identification of patients at risk of severe APOP and PPP for their effective and safe management, both in the hospital and at home (16).
All cases with unsuccessful treatment of APOP in the hospital ward (numerical scale larger than 6), patients with chronic pain requiring high doses of opioids or patients with substance abuse should have multidisciplinary care through a pain doctor. This care should begin preoperatively, continue after the surgery, and finally after discharge from hospital (13). The early identification of these complex patients and their timely and appropriate management would make it possible to reduce the chronic use of opioids and the incidence of PPP (13,15,17).
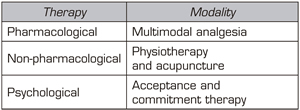
For this purpose, the TPC or TPS were created. An TPS or TPC is a novel program that aims to effectively manage APOP, facilitate opioid weaning, reduce the development of chronic pain disability, and help decrease deaths related to opioid overprescription (18). These units were created to effectively manage patients’ perioperative pain, maintain function, reduce opioid use, and monitor the efficacy of these interventions. In 2014, the first program of this type was organized, which focuses on the PPP in three stages: 1) pre-operative, 2) postoperative in the hospital setting, 3) postoperative in the outpatient setting up to 6 months after surgery (13,19).
The services offered by the TPC are divided into three categories (13) (Table I):
Table I. Individualized treatments provided by transitional pain services (TPS)
Two types of patients are treated in TPS (22):
This is managed through an interdisciplinary team consisting of anesthesiologists, acute pain nurse practitioners, clinical psychologists, palliative care specialists, an exercise physiologist, and a patient care coordinator (19). These units allow the early detection of patients with risk factors for PPP and timely therapeutic and psychological medical interventions to reduce the transition to chronic pain and reduce dependence on opioids (17). Shorter hospital stays, early weaning from opioids, less emotional distress, better quality of life, lower incidence and severity of PPP and disability, and substantial savings are achieved in this way (17).
These units serve as intermediaries between the treatment of APOP in the inpatient ward and the management of chronic outpatient pain. There, patients that could present with chronic pain will be identified among hospitalized patients, based on prognostic indicators (15). The patient should visit the TPC after the discharge. At the TPC, the formulated treatments are reviewed, the patient’s treating physician is contacted for the corresponding surgical review, and the patient is referred to other services, such as physical medicine and rehabilitation, mental health, addiction medicine and multidisciplinary services of chronic pain if necessary. This behavior should identify, treat and modify the pain course of patients with a higher risk of PPP and of excessive opioid use (13,17,23). The operation of a TPC is shown in Figure 1.
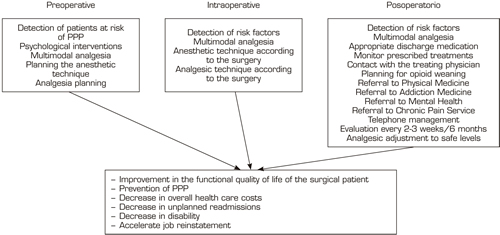
Fig. 1. Operation of a transitional pain clinic (TPC).
A TPC conceived in this way will allow (15):
The criteria for referral to the TPS are varied (13,16,22) (Table II).
Risk factors for PPP to be considered in the TPC, TPS or acute pain services (APS).
Table II. Criteria for referral to the transitional pain clinic (TPC)
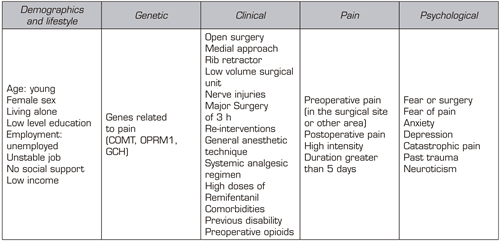
Five categories of risk factors for PPP have been identified: demographic, genetic, clinical, related to surgery and psychological, only four of them can be measured with validated tools (pain, physical functioning, psychological functioning and global score of the result (15,16, 24,25,26) (Table III).
Table III. Persistent postoperative pain (PPP) risk factors
The TPS is the first service that comprehensively addresses the problem of PPP after major surgery through multidisciplinary care that begins preoperatively, extends post-operatively, and continues until the period of discharge from hospital once patients have returned home. The main objectives of the TPS are: 1) To provide a novel and uninterrupted approach to pre- and postoperative pain management for patients at higher risk of developing PPP and pain disability, 2) To manage opioid medications for medically complex patients after discharge, and 3) improve management and functioning of the patient to guarantee the best possible quality of life after surgery (13).
As an example of this modality of pain services we will mention the TPS of the Toronto General Hospital. Structurally, it consists of five anesthesiologists with advanced training in acute and chronic interventional pain, two clinical psychologists, two physiotherapists with experience in acupuncture, a palliativist family doctor, a patient care coordinator, and an administrative assistant (13).
When patients are discharged, they are evaluated at 2-3 weeks or sooner in the TPS if needed. The patient’s progress regarding pain and opioid weaning plans are evaluated. This evaluation is performed every 2-3 weeks, and among other aspects, analgesics are adjusted until the patient is at a safe level, patient’s pain is under control and patient’s activities of daily living are close to their preoperative level.
The TPS is designed to address the historic gap in pain management of the surgical patient by providing continuous care preoperatively, during hospital stay, and on discharge home after hospital discharge. These stages are relevant in the prevention of PPP, reducing hospital stay, readmissions, opioid consumption and general costs for medical care. However, we must not overlook that we are in the COVID-19 pandemic. This new situation demands innovations in medical care and it is time to look for alternatives to the conventional choices for the follow-up of patients, it is time forTelehealth. Telehealth encompasses the use of telecommunications to provide health care, patient education, and public health (18). With the pandemic situation, restrictions on non-urgent medical care are imposed, TPS consultations are limited, being the use of existing technologies, such as telephone, FaceTime, Skype, Zoom or other platforms for video conferences, an option to reduce this barrier. The COVID-19 pandemic forces social distancing, but we must leverage video telehealth and TPS to continue monitoring our patients (18). Patients, through mobile applications, can collaborate in their self-assessment of pain scores, which facilitates their follow-up and their active participation in pain management (27).
REFERENCES