DOI: 10.20986/resed.2022.3956/2021
ORIGINAL
END-OF-LIFE TRANSFUSIONS IN PATIENTSWITH AN ONCOLOGICAL DIAGNOSIS
TRANSFUSIONES AL FINAL DE LA VIDA EN PACIENTESCON DIAGNÓSTICO ONCOLÓGICO
A. P. Brome Uribe1
L. M. Martínez Sánchez1
L. Herrera-Almanza1
M. Fonseca-Guzmán1
C. Durango-Sánchez1
V. Vasquez-Estrada1
L. Duque-Echeverri1
A. Morales-Montoya1
M. E. Saavedra-Valencia1
J. F. Vargas-Silva2
S. M. Molina-Giraldo3
1Facultad de Medicina. Universidad Pontificia Bolivariana. Medellín, Colombia
2Hospital Pablo Tobon Uribe Hospital. Medellín, Colombia
3Clínica Vida. Medellín, Colombia
ABSTRACT
Introduction: Cancer patients in terminal stages present symptoms related to anemia, other cytopenias, and coagulopathies that deteriorate the quality of life. These symptoms can be multicausal and do not improve in most cases.
Objective: Describe the use of blood transfusions in the six months before death as an alternative palliative treatment in patients with an oncological diagnosis in the city of Medellin during the period 2013-2018.
Methods: Retrospective cohort, in patients with a cancer diagnosis who received transfusions in the last six months of life, a non-probabilistic sampling of consecutive cases was executed. The analysis was carried out in SPSS, estimating absolute and relative frequencies and median with interquartile ranges.
Results: Out of 3,254 medical records of cancer patients, 151 were included. The time to oncological diagnosis had a median of 2 years (IQR 1 and 3). The symptoms observed in patients before and after the first transfusion were pain, present in 32.1 % (46) and 16.9 % (25) respectively, besides drowsiness was distinguished in 25 % (36) before transfusion and 14.3 % (21) after. Finally, the clinical outcomes before and after the last transfusion prior to death, were a decrease in pain, asthenia/adynamia, drowsiness, among others.
Conclusions: The findings of this research allow us to appreciate the current panorama in the institutions in which palliative care medical services are being provided and consider when to offer the blood products to a patient at the end of life as a therapeutic measure in the context of a human being cared by physicians.
Key words: Blood transfusion, hospice care, quality of life, cancer, pain
RESUMEN
Introducción: Los pacientes con cáncer en fase terminal presentan síntomas relacionados con la anemia, otras citopenias y coagulopatías que deterioran la calidad de vida. Estos síntomas pueden ser multicausales y no mejoran en la mayoría de los casos.
Objetivo: Describir el uso de transfusiones sanguíneas en los seis meses previos a la muerte como alternativa de tratamiento paliativo en pacientes con diagnóstico oncológico en la ciudad de Medellín durante el periodo 2013-2018.
Métodos: Cohorte retrospectiva, en pacientes con diagnóstico de cáncer que recibieron transfusiones en los últimos seis meses de vida, se ejecutó un muestreo no probabilístico de casos consecutivos. El análisis se realizó en SPSS, estimando frecuencias absolutas y relativas y mediana con rangos intercuartílicos.
Resultados: De 3254 historias clínicas de pacientes con cáncer, 151 fueron incluidas. El tiempo hasta el diagnóstico oncológico tuvo una mediana de 2 años (IQR 1 y 3). Los síntomas observados en los pacientes antes y después de la primera transfusión fueron el dolor, presente en el 32,1 % (46) y el 16,9 % (25) respectivamente, además de la somnolencia que se distinguió en el 25 % (36) antes de la transfusión y el 14,3 % (21) después. Finalmente, los resultados clínicos antes y después de la última transfusión antes de la muerte, fueron una disminución del dolor, astenia/adinamia, somnolencia, entre otros.
Conclusiones: Los hallazgos de esta investigación permiten apreciar el panorama actual en las instituciones en las que se prestan servicios médicos de cuidados paliativos y considerar cuándo ofrecer los hemoderivados a un paciente al final de la vida como medida terapéutica en el contexto de un ser humano atendido por los médicos.
Palabras clave: Transfusión sanguínea, cuidados paliativos, calidad de vida, cáncer, dolor
Correspondencia: Lina María Martínez-Sánchez
linam.martinez@upb.edu.co
Recibido: 02-11-2021
Aceptado: 21-02-2022
INTRODUCTION
Cancer patients in terminal stages present symptoms related to anemia, other cytopenias, and coagulopathies that deteriorate the quality of life (1,2). These symptoms can be multicausal and do not improve in most cases with a single medical intervention (1,3).
The search, description, and study of procedures or therapies used by the health care team at the end of life allow to nurture the literature focused on patients that receive palliative cares, and know the benefits of supportive care, including reduced health care costs, symptomatic control, and decision making tailored to the biopsychosocial needs of patients (4).
When we want to provide the cancer patient with a therapeutic option to extend survival or achieve remission, we can resort to transfusion of blood products. These is a unique palliative alternative, whose objective is focused on the comfort and well-being of the patient, improving their quality of life (2).
It is important to know the clinical characteristics, comorbidities, time of diagnosis, and therapeutic needs of terminal cancer patients to make future approaches based on the use or not of blood products at the end-of-life context. In addition to being a vulnerable population, there are ethical, legal, and procedural doubts about a finite resource that requires a multidimensional approach (5,6).
The worldwide prevalence of cancer is increasing in underdeveloped countries, which currently account for 82 % of the total population diagnosed with cancer, and 70 % of cancer-related deaths globally (7).
Anemia is common in palliative care patients with a reported hospital prevalence of 50 % for any admission and 90 % for the last hospitalization before death, with prevalence of 77 % in men and 68 % in women (8). Among the patients who have received a blood product as palliative treatment for improve the anemia and its associated symptoms, is estimated that between 31 % and 70 % had a transitory benefit lasting approximately two weeks (8-10).
The paucity of literature describing the quantity, usefulness, and effectiveness of blood transfusions, and especially in palliative care patients, is presented as a difficulty when it comes to consideration the indications for blood product therapy in palliative care patients (1,5,11,12).
Therefore, the objective of the study was to describe the use of blood transfusions in the six months before death as an alternative palliative treatment, in patients with an oncological diagnosis in the city of Medellin during the period 2013-2018.
METHODS
A retrospective cohort study was conducted, including patients with an oncologic diagnosis who received blood transfusions for palliative purposes during the six months prior to their death. Eligibility criteria were pediatric and adult patients, who died between 2013 and 2018, cared for in the participating institutions. A non-probabilistic sampling of consecutive cases was executed.
The primary source of data collection was the medical records of patients who met the eligibility criteria. A survey designed included all the sociodemographic, clinical, and transfusion variables necessary to fulfill the proposed objectives. The collected information was stored in a database.
The data analysis was run using the software SPSS version 24, with adequate availability of both quantitative variables (median with interquartile ranges) and qualitative variables (absolute and relative frequencies expressed as proportions and percentages).
This study was approved by the Health Research Ethics Committee of the Universidad Pontificia Bolivariana and the participating institutions.
RESULTS
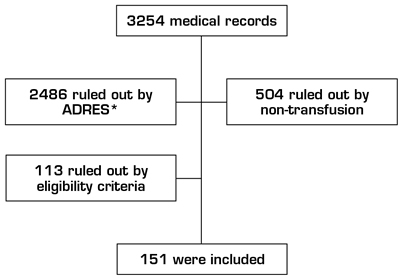
Out of 3254 medical records of cancer patients, were included 151, of which 78 (51.7 %) were male, with a median age of 64 years of age (IQR 52-75). The median time of oncologic diagnosis was two years (IQR 1 and 3) (Figure 1).
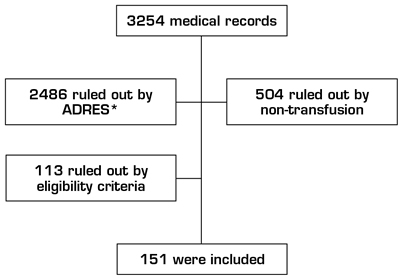
Fig. 1. Patient selection. *ADRES Administrator of Resources of the General Social Security Health System.
Regarding the International Classification of Diseases -10 (ICD 10), the most frequent diagnosis was C189 corresponding to a malignant tumor of the colon, unspecified part with 6.6 % (10), followed by C169, malignant tumor of the stomach, C833, diffuse large B-cell lymphoma, both with 4 % (6).
Of the patients included in the study, 62.3 % (94) were outpatients and 37.7 % (57) hospitalized.
In the hemoclassification of the patients included in the study, O+ 53 % (80), A+ 31.2 % (47), B+ 6 % (9), O- 4.6 % (7), A- 2.6 % (4), AB+ 1.3 % (2), ND 1.3 % (2) was reported.
About the pathological background, was found that the most frequent were arterial hypertension with 34.4 % (52), followed by diabetes mellitus 13.2 % (20) (Table I).
Table I. Patients’ pathological background.
*Non-exclusive.
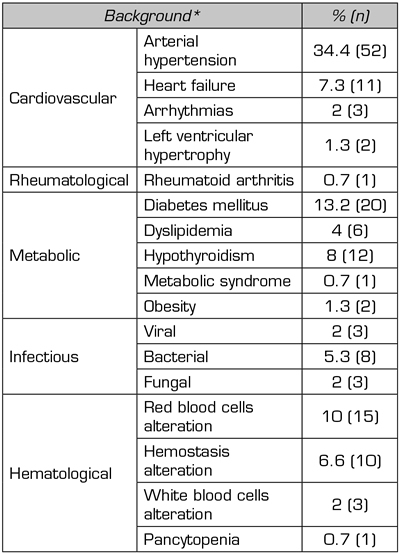
The most frequent primary tumor was found in the gastrointestinal system with 40.4 % (61), followed by the hematopoietic system with 29.8 % (45) (Table II).
Table II. Location of primary cancer.
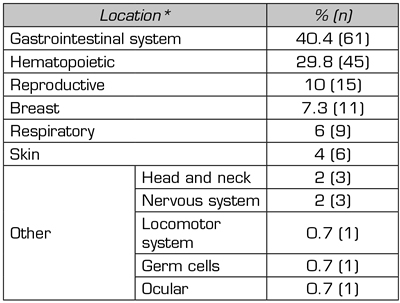
*Non-exclusive.
The reported presence of metastases was in 48.3 % (73) of the patients.
Concerning to the treatment for oncological pathologies, patients received: chemotherapy, surgery, radiotherapy, and immunotherapy with 62.9 % (95), 42.4 % (64), 12.6 % (19) and 2.7 % (4) respectively. 81.6 % (111) required therapeutic modification at some point after diagnosis.
Palliative treatment with blood product was used in the study patients during the six months before their death, with a median of 261.5 cubic centimeters (cc) (IQR 242 - 293) of blood product doses and a median of 1 unit (IQR 1-2) transfused per patient (Table III).
Table III. Characterization of blood products.
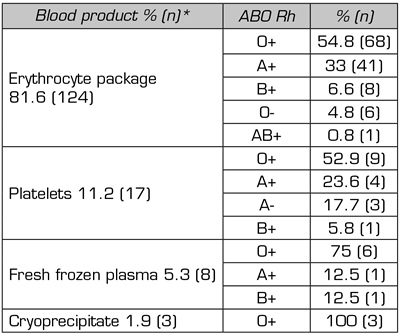
*Non-exclusive.
The blood products are used to improve the clinical condition of patients in palliative care and impact their quality of life. With transfusions received during the last six months preceding death, changes were noted in the hemoglobin values before and after the first transfusion, with 8.5 g/dL (IQR 7-10.4) 10 g/dL (IQR 9.3-10.5) respectively. In the last transfusion the values were 8 g/dL (IQR 7-8) (Table IV).
Table IV. Pre and post-transfusion paraclinical tests.
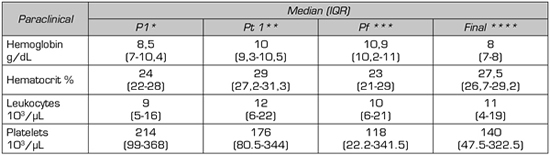
*P1 before the first transfusion. **Pt1 after the first transfusion. ***Pf before the last transfusion. ****Final.
The symptomatology presented by the patients before and after the first transfusion were: pain; present in 32.1 % (46), and 16.9 % (25) respectively. Same was observed with drowsiness in 25 % (36) and 14.3 % (21) before and after, respectively (Table V).
Table V. Pre and post-transfusion symptoms for the first transfusion.
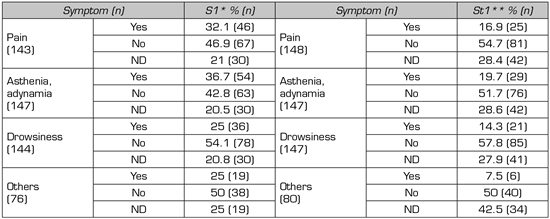
*S1 before the first transfusion.
*St1 after the first transfusion.
The symptoms observed in patients before and after the last transfusion prior to death, were a decrease in pain, asthenia/adynamia, drowsiness, among others (Table VI).
Table VI. Pre and post-transfusion symptoms for the last transfusion.
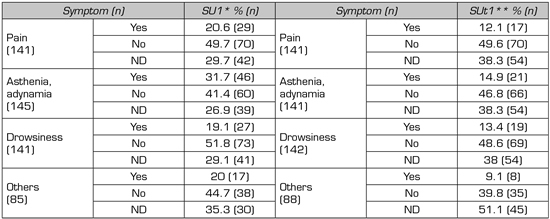
*SU1 before the first transfusion.
*SUt1 after the first transfusion.
Discussion
Quality in end-of-life care in low incomes countries has been focused on the analysis of macro indicators such as the existence of palliative care policies, per capita morphine consumption and the number of medical schools that include training programs in palliative care, hence off, it is still necessary to establish interdisciplinary management guidelines for these patients (13).
In the study led by Goksu et al. (9), in Turkey with oncological patients, reported that the predominant sex was male with 62.3 % and a median age of 61 years of age, comparable data to the present study in which 51.7 % corresponding to the male sex with a median age of 64 years. While, Soares et al. (13) in Brazil reported a median age of 63 years and a female predominance of 61 %. Also, Moracchini et al. (14) reported in a study performed in France a median age of 68 years and a male predominance of 51 %.
Out of the patients included in the study, 62.3 % (94) were handled as outpatients and 37.7 % (57) as inpatients. Compared to the study conducted by Soares et al. (13) in which 62 % (536) were reported to have gone to the emergency room, and 33 % (288) were admitted to the Intensive Care Unit (ICU).
Moracchini et al. (14) reported a median time of oncologic diagnosis of one year and two months, comparable to that of the present study, which reported a median of 2 years.
In respect of the location of the primary tumor, Soares et al. (13) reported 26 % (217) breast and 13 % (109) lung, compared to the present study, the gastrointestinal system was more frequent with 40.4 % (61), followed by hematopoietic with 29.8 % (45). On the other hand, in the study by Goksu et al. (9), was reported that the most common were lung 27 % and pancreas/biliary tract 10 %.
In the study by Sandgren and Strang (15) conducted in Sweden on cancer patients, was reported that 17.1 % of patients required radiotherapy and 10 % surgery, in comparison with this study in the one 42.4 % and 12.6 % required surgery and radiotherapy, respectively.
Platelet transfusions are commonly used to prevent or stop spontaneous bleeding in thrombocytopenic patients with hematological malignancies. The complexity of decision-making may be greater in patients at the end of life, in clinical, structural, and ethical aspects. In addition, Moracchini et al. (14), reported that the management of platelet transfusion at the end of life follows a case-by-case policy, based on low-level evidence only, such as expert opinion or retrospective analysis.
In comparison to this research, in which 11.2 % of patients received platelet transfusions, Goksu et al. (9)reported that about 13.8 % of patients received this blood product. Also, in a study performed in Germany by Wandt et al. (16), 75 % of cancer patients received platelet concentrate. The therapeutic indication for this blood product is to stop active bleeding due to thrombocytopenia as prophylaxis for bleeding, knowing that this type of therapy is an issue in patients with advanced cancer.
Red blood cell transfusions in palliative care patients require a careful, mechanism-based approach that considers the patient’s context, comorbidities, prognosis, and care targets (8). In this research, 81.6 % of the patients received red blood cell transfusion, compared to the work done by Goksu et al (9), in which 38.4 % of the patients included in the study received this specific therapy.
As for the change in the before and after transfusion hemoglobin value, a study by To et al (17) reported an average pre- and post-transfusion hemoglobin of 7.8 g/dL and 10.1 g/dL, in comparison, with this study in which average pre-transfusion was 8.5 g/dL and post-transfusion of 10 g/dL. On the other hand, in the study conducted by Goksu et al. (9), the average pre-transfusion hemoglobin reported was 9.9 g/dL. This measure was obtained after the first transfusion and shows an improvement in this parameter thanks to the implementation of blood as palliative therapy.
Concerning the information above, the hemoglobin values reported in this study were 10.9 g/dL before and 8 g/dL after transfusion. A significant drop is observed in this parameter since this intervention was performed on the days close to death.
Goksu et al. (9), reported that cancer-related fatigue is the most prevalent symptom, occurring in 5 %-90 % of patients, which severely impacts their quality of life and functional capability; compared to the current study in which the presence of fatigue before the first transfusion and before the last transfusion was present in 36.7 % and 31.7 % of patients, respectively. In another study conducted by To et al. (8), the primary symptoms presented in patients who were going to receive red blood cell transfusion were: fatigue in 83 %, dyspnea in 29 %, generalized weakness in 13 %, dizziness in 7 %, and other symptoms in 8 %. On the other hand, the author Mercadante et al. (18) reports that previous studies stated significant changes in fatigue and dyspnea found immediately after transfusion, although the effect was partially lost 15 days after transfusion.
The literary reference on quality end-of-life care was elaborated in academic centers situated in high-income and developed countries, with better practice management than in Colombia. For this reason, the findings may be useful in countries with limited resources, since they represent a realistic scenario adapted to the economic and political situations of Latin America, which facilitates the formulation of health strategies and policies that guarantee adequate decision making for the care of these patients (9,13,14).
Finally, terminal patients who received a blood product transfusion showed an improvement in their symptoms. From this, it can be assumed that blood transfusions should not be denied to patients with neoplasms in palliative care however, the use of blood transfusions in terminal cancer is a therapy for which there is little literature available. Therefore, more research is required to define the role of transfusions in terms of survival, improvement of symptoms, and quality of life in these patients, as well as to consider aspects such as the opinion of family members, expectations of patients, and criteria of health professionals (9,13,14).
The limitations found in the study were evidenced in the data collection process due to the lack of available data in the medical records, especially regarding pre-and post-transfusion paraclinical and symptoms. Therefore, at the time of analyzing the results, the sample size was affected because they did not meet the selection criteria, and post-transfusion complications were not evident in the data obtained, since the transfusions had other therapeutic objectives.
CONCLUSIONS
This research allows us to appreciate the current panorama in the institutions that provides palliative care medical services and consider when to provide transfusion blood products to a patient at the end of life as a therapeutic measure in the context of a human being cared for by physicians.
REFERENCES