DOI: 10.20986/resed.2021.3837/2020
ORIGINAL
PHARMACOLOGICAL OSTEONECROSIS IN MAXILLOFACIAL SURGERY, PERIOD 2013-2019
OSTEONECROSIS FARMACOLÓGICA EN CIRUGÍA MAXILOFACIAL, PERIODO 2013-2019
A. G. Juárez Rebollar1
A. Colín Ordaz2 y D. Juárez Rebollar3
1Maxillofacial Surgery Service. Specialty Hospital Dr. Bernardo Sepulveda Gutiérrez National Medical Center. Siglo XXI, IMSS. Mexico
2Neurosurgery Service. Adolfo López Mateos Regional Hospital. Mexico
ABSTRACT
Introduction: The word osteonecrosis (ONC) means “dead bone”; it is a bone disease secondary to the loss of blood supply to the bone, causing its collapse and subsequent death. It can occur in any bone in the body, including those of the maxillofacial region, it is more common in the jaw. In recent years, the relationship of ONC with drugs such as bisphosphonates, antiresorptive, steroids for prolonged use, angiogenesis inhibitor agents, among others, has been found. However, despite the studies carried out by various authors, ONC continues to be an underdiagnosed entity with variable management and treatment, which is why the interest of this research arises with the main objective of reporting the cases of patients diagnosed with Pharmacological ONC.
Material and method: A descriptive, retrospective, cross-sectional, observational study was carried out for approximately 6 years (January 1, 2013 - December 31, 2019), in the Maxillofacial Surgery service of the Specialty Hospital, of National Medical Center, “Siglo XXI”, IMSS. Making a review of clinical records, collecting clinical and image controls, reporting the number of cases and the management of patients with ONC, as well as the number of cases of ONC that were related to drugs. Of 9 patients with a diagnosis of osteonecrosis (ONC), only 4 patients were Pharmacological ONC, from the Maxillofacial Surgery service.
Results: From a universe of 9 patients with ONC, 4 representative cases of patients with pharmacological ONC were presented, with management based on the protocol used in the Maxillofacial Surgery service of the National Medical Center “Siglo XXI”, IMSS; Likewise, the signs and symptoms with which the treatment was staged and determined are shown. The pharmacological treatment associated with ONC was: in 3 patients bisphosphonates (zoledronic acid) and only one patient with Denosumab. The most frequently affected site was the mandible and only one case was bimaxillary (maxilla and mandible). The treatment used as stipulated according to the case, in two ways: conservative and surgical, in both cases a 0.12 % chlorhexidine-based mouthwash was added, and only in case of the presence of infection amoxicillin-based antibiotic with clavulanic acid was given.
Discussion: The present study was carried out only in the Maxillofacial Surgery service of the National Medical Center, “Siglo XXI”, IMSS. The stages were differentiated according to the AAOMS, SICMF, and SIPMO, clinically imaging. The importance of carrying out a study exclusively of the Maxillofacial Surgery service will allow providing more specific information on the area to later study ONC jointly and in a multidisciplinary way, to later carry out more extensive reports of pharmacological osteonecrosis and/or bisphosphonates, in addition to later elaborating multicenter studies.
Key words: Osteonecrosis, pharmacological, bisphosphonates, denosumab.
RESUMEN
Introducción: La palabra osteonecrosis (ONC) significa “hueso muerto”. Es una patología ósea secundaria a la pérdida de suministro de sangre al hueso, provocando su colapso y su posterior muerte. Puede presentarse en cualquier hueso del cuerpo, incluyendo los de la región maxilofacial; es más frecuente en la mandíbula. En los últimos años se ha encontrado la relación de la ONC con medicamentos tales como bifosfonatos, antirresortivos, esteroides por uso prolongado, agentes inhibidores de angiogénesis, entre otros. Sin embargo, pese a los estudios realizados por diversos autores, la ONC continúa siendo una entidad subdiagnosticada y con manejo y tratamiento variable; es por ello que surge el interés de esta investigación con el principal objetivo de reportar los casos de pacientes diagnosticados con ONC farmacológica.
Material y método: Se realizó un estudio descriptivo, retrospectivo, transversal, observacional, durante aproximadamente 6 años (1 de enero de 2013- 31 de diciembre de 2019), en el servicio de Cirugía Maxilofacial del Hospital de Especialidades, del Centro Médico Nacional, Siglo XXI, IMSS. Haciendo una revisión de expedientes clínicos, recabando controles clínicos y de imagen, reportando el número de casos y el manejo de pacientes con ONC, así como el número de casos de ONC que estuvieron relacionados a fármacos. Se obtuvo una muestra de 9 pacientes con diagnóstico de osteonecrosis (ONC) en el Servicio de Cirugía Maxilofacial.
Resultados: No se encontró predominio por algun género en específico, la edad promedio fue de 63,44 años, aproximadamente el 50 % de la muestra obtenida fueron pacientes diagnosticados con ONC farmacológica, de los cuales solo uno estuvo asociado a denosumab y 3 fueron ONC relacionada con bifosfonatos. El tratamiento empleado se estipuló acorde el caso, por dos formas: conservadora y quirúrgica; en ambos casos se agregó colutorio a base de clorhexidina al 0,12 % y solo en caso de presencia de infección se dio antibiótico a base de amoxicilina con ácido clavulánico.
Discusión: El presente estudio se realizó únicamente en el servicio de Cirugía Maxilofacial, del Centro Médico Nacional, Siglo XXI, IMSS. Se clasificaron los estadios conforme a la AAOMS, SICMF and SIPMO, clínico-imagenológicamente. La importancia de realizar un estudio exclusivamente del Servicio de Cirugía Maxilofacial brindará información más específica del área para posteriormente abordar de manera conjunta y multidisciplinariamente la ONC y poder realizar reportes más amplios de la osteonecrosis farmacológica y/o en relación a bifosfonatos, además de dar pie a realizar posteriormente estudios multicéntricos. Es por ello que en este trabajo se partió de lo específico para posteriormente ampliar el campo de estudio.
Palabras clave: Osteonecrosis, farmacológica, bifosfonatos, denosumab.
Received: 30-07-2020
Accepted: 23-08-2021
Correspondence: Alejandra Giselle Juárez Rebollar
giselle_juarez@hotmail.com
INTRODUCTION
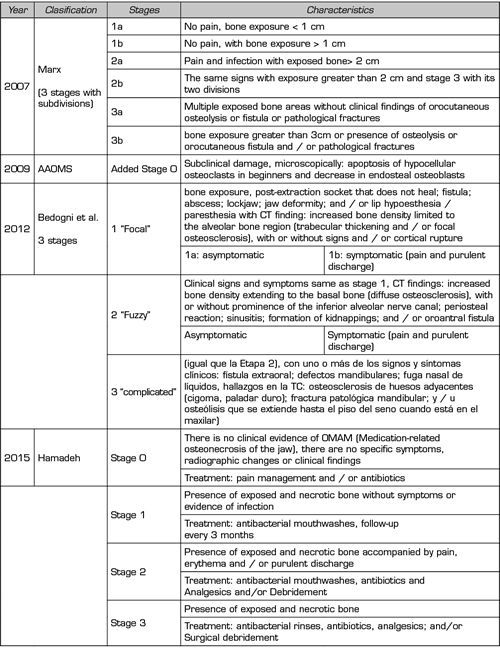
Some bone pathologies such as osteonecrosis (ONC) have been associated with the administration of medications, including bisphosphonates (1). The reports are from patients with a history of cancer, other diseases such as osteoporosis, Paget’s disease, hypercalcemia, among others (1,2). Bisphosphonates (BP) are associated with the presence of some cases of ONC in the maxillofacial region, as mentioned by Bilezikian (3,4)and Ruggiero (5,6) among other authors; which can occur during or after therapy with these drugs (BP), mainly intravenously way, among the most widely used are pamidronate and zoledronate (4,5) Another drug associated with ONC is Denosumab, steroids for a long time and/or angiogenesis inhibiting agents (7,8). ONC in the maxillofacial region may or may not present clinical bone exposure (1,9-13). Other clinical data is the presence of pain (patients with an oncological history and/or metastatic), the risk of infection, increased bone fractures (pathological) that may require surgical and/or palliative management, when it occurs in relation to the spine, can compress the spinal cord that may result in paresthesias, incontinence and paralysis, etc. (2,3). In 2014, the American Association of Oral and Maxillofacial Surgeons (AAOMS) defined Osteonecrosis (ONC) as exposure of necrotic bone in the maxillofacial region that lasts more than 8 weeks, when a patient has been treated with antiresorptives (denosumab) or antiangiogenic agents and the patient has had no antecedent of radiation therapy to the head and neck (5). Previously, this condition (ONC) was only associated with bisphosphonates; however, the term “related to drugs” was introduced when its associated with other drugs. Ruggiero et al., in 2006, mention three stages based on signs and symptoms (6). One year later (2007), Marx divided the stages according to the size of the lesion (14). In 2009, the AAOMS added Stage 0 (zero) (6); then in 2012 Bedogni et al. (14) mention the clinical-radiological staging (14,15). In 2015 Hamadeh refers to the characteristics of ONC in the maxillary and mandible region as well as the treatment that is suggested in each of the 4 stages (stage 0-3) (Table I). The Italian Society of Maxillofacial Surgery (SICMF, 2012) and the Italian Society of Oral Pathology and Medicine (SIPMO) (14) proposed a new definition of osteonecrosis: is an adverse pharmacological reaction with destruction and progressive bone death, affecting the mandible or maxilla in patients exposed to nitrogen-containing BP treatment, without prior radiation therapy, approximately 76 % of ONC due to BP were diagnosed and 24 % did not present non-visible necrotic bone, therefore it could not be diagnosed (14). Bisphosphonates are small molecules that dock at hydroxyapatite binding sites in bone, osteoclasts reabsorb bisphosphonate-impregnated bone, and released BFs bind farnesyl pyrophosphate synthase inside osteoclasts. producing an apoptosis (7,18,19).
On the other hand, denosumab is an anti-resort type: human IgG2 monoclonal antibody (non-chimeric), which has high affinity and specificity when binding with the nuclear factor activator receptor kappa-B ligand (RANKL), therefore prevent the activation of its RANK receptor on the surface of osteoclast and osteoclast precursors, it will inhibit the formation, function and survival of osteoclasts by preventing RANKL/RANK interaction, causing a decrease in bone resorption (20,21). It is also used to treatment of patients diagnosed with osteoporosis, mainly in postmenopausal women, reduce bone loss as a result of breast cancer treatment, use to prevent bone loss associated with hormonal decline in men diagnosed with prostate cancer (22). The incidence of bisphosphonate-induced ONC (1-18.6 %), in the maxillo-mandibular region, is higher than denosumab ONC (approximately 2 % in patients with metastatic bone disease and less than 0.01 % in patients treated for osteoporosis) (8,23-26). Treatment can be of two types, the treatment can be of two types, depending on the signs and symptoms: type 1 conservative (local oral hygiene measures, rinses with chlorhexidine and in cases of infection, culture and subsequent antibiotic therapy and even hyperbaric chamber or other therapies) and type 2: Surgical management (includes curettage, decortication, osteotomies with their respective reconstruction) (8,27). In recent research such as Hamadeh in 2015 refers to the characteristics of ONC in the maxillary and mandible region, as well as the treatment that is suggested in each of the 4 stages (stage 0-3) (Table I) (16,17).
Table I. Different classifications of the onc according to stages and characteristics (6,14-17)
Objectives
Report the patients who present pharmacological osteonecrosis (ONC), in the Maxillofacial Surgery of the National Medical Center, “Siglo XXI”, of the Mexican Institute of Social Security (IMSS), Mexico City for 6 years, from January 1st 2013 to December 31st 2019. Likewise report the management that was given to patients with a diagnosis of pharmacological osteonecrosis in the Maxillofacial Surgery service.
MATERIAL AND METHODS
An observational, retrospective, descriptive study was carried out for 6 years on “Pharmacological osteonecrosis in Maxillofacial Surgery”, from the National Medical Center, “Siglo XXI”, IMSS. From January 1st 2013 to December 31st 2019. A review of clinical records, corroborating clinical data of patients under control by the Maxillofacial Surgery service, collecting pathological personal history, age, gender, medication, previous management, location of osteonecrosis and its treatment.
The inclusion criteria were: patients treated in Maxillofacial Surgery, from the National Medical Center, “Siglo XXI”. From January 1st 2013 to December 31st 2019, with diagnosis pharmacological osteonecrosis, any gender regardless of personal pathological history, patients with intra or extraoral lesions associated with pharmacological osteonecrosis, patients taking biphosphonates or who are undergoing treatment for diseases with bone resorption, such as osteoporosis and cancer with bone metastases.
The exclusion criteria were: patients treated in other medical units or services, with no diagnosis of pharmacological osteonecrosis, minors, or previous post-surgical sequelae, patients who present osteonecrosis for other non-drug causes, such as radiotherapy, for complications or sequelae of other conditions not associated with drugs, patients with a diagnosis other than osteonecrosis.
Analysis of data
A specific statistical test was not used since only an observational and descriptive study was carried out, in addition to the fact that the sample is very small, the statistical program SPSS 14 was used as support and an analysis was carried out based on frequencies.
RESULTS
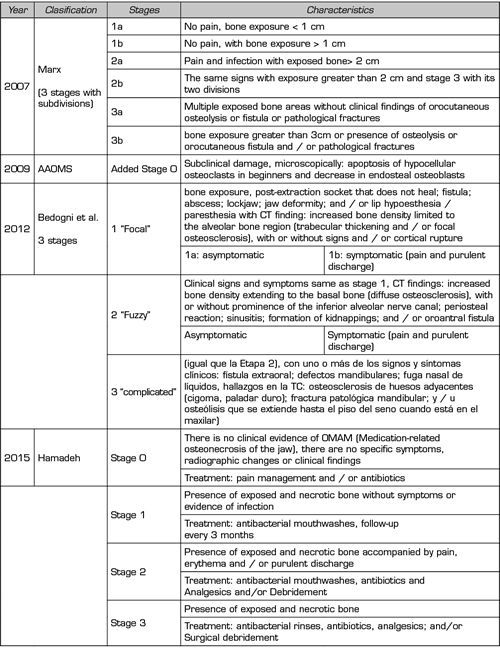
In a period of approximately 6 years 6 years (January 1, 2013 - December 31, 2019), the following results are reported: analyzing first in a general way and later in a specific way. The results of the frequency of patients with a diagnosis of ONC (regardless of the etiology) were a total of 9 cases of which 5 were women and 4 men, The ranges of age was: minimum ranges: 51 years and maximum 78 years, 8 of these patients had lesions in the mandible and the remaining case bimaxillary (mandible and maxilla). Only 4 patients presented all the inclusion criteria and the main diagnosis of “pharmacological osteonecrosis” of which 3 patients were related to the use of bisphosphonates (zoledronic acid) and 1 patient with denosumab (diagnosis of osteoporosis). The most frequent affected site was the mandible (3) and only one case was bimaxillary (maxilla and mandible). Mention that the other patients who did not meet all the inclusion criteria and were not related to medications (these 3 excluded cases were not caused by drugs but by other causes such as trauma, infection, previous surgeries with complications and altered healing that is). The 4 cases of patients who presented pharmacological ONC Table II, underwent surgery with an initial decortication. 1 patient had decortication with subsequent surgical lavage in a second surgical period, 1 patient had decortication and in a second period required ostectomy and mandibular reconstruction with titanium plate. 1 patient required in bloc resection in the maxilla and mandible, subsequently underwent closure of orocutaneous fistulas, and 1 patient was first subjected to surgical lavage, later, when presenting a localized opportunistic infection, canalization and drainage was performed, decortication, another curettage, then surgical lavage, required vacuum-assisted therapy, and finally the wound was allowed to close by second intention. In general, of all patients with osteonecrosis (regardless of the origin), the most used management was decortication, followed by surgical lavage and curettage (Figure 1). Mouth rinses with 0.12 % chlorhexidine, strict oral and body hygiene (daily bath), amoxicillin-based antibiotic with clavulanic acid 500 mg/125 mg, treatment time was variable, depending on the case and the clinical characteristics of the lesions, the schemes used were 14 days, 21 days and a month; in those cases in which he had an active infection (exudate of any type and/or pus) it was prescribed for up to 21 days or a month, in the rest for two weeks. The period of observation, control, management and evolution of all patients from the moment of their management by the maxillofacial surgery service was approximately 10 months to a year and a half, so that the clinical lesions remitted in relation to ONC. Of the 9 cases, only 2 were serious considering that the patients had a history of long-term management with bisphosphonates (zoledronic acid) and that they had previously received dental care as part of a preventive protocol. These 2 patients were those who required mandibular and maxillary block resection and the other was the one who required reconstruction with a titanium plate. In relation to the clinical characteristics presented by the 4 patients with pharmacological ONC. The youngest patient (1) was diagnosed in another clinic when they carried out a molar extraction and there was a delay in healing of more than 3 weeks, clinically he had a denuded area painful on palpation in the molar region. He was the patient who required the least surgeries and improved the fastest (14 days). The oldest patient (2) had a millimeter denuded area, she did not report symptoms, however, by tomography an affected area of ??2.5 cm was found, she underwent an initial decortication (as in all patients), followed by an Ostectomy and subsequently performed a Reconstruction (with Titanium Plate) of the mandibular bone defect. The third patient was the only one who underwent Bloc resection in the maxilla and mandible, the defect in this patient was wide, clinically she did not present a denuded bone area, but if she had a fistula in the distal premolar region, tomographically it presented a defect broad diffuse non-limited bone spanning from the alveolar border with extension to the mandibular basal border being of great thickness, Subsequently repair of orocutaneous fistulas. And the fourth patient clinically presented a small fistula of approximately 5 mm but referred diffuse pain in the mandibular border for no apparent reason, a tomography was performed and a diffuse area was found in the mandibular body and mandibular symphysis, this patient was the one who underwent More number and types of treatments, the first antimicrobial scheme was with amoxicillin with clavulanic acid (21 days), during the course of his treatment he presented a secondary infection, therefore, according to the antibiogram performed, treatment with clindamycin was started (14-day scheme) and later the antibiotic with amoxicillin with clavulanic acid was restarted again (1 month) reporting adequate evolution, at the end with adequate wound healing and fistula (closure by second intention).
Table II. Presentation of cases of pharmacological onc of maxillofacial surgery, at national medical center "siglo XXI". Period 2013-2019
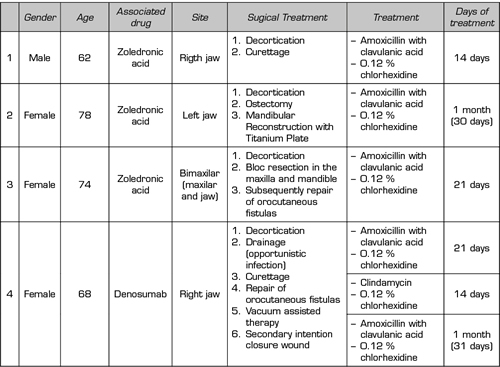
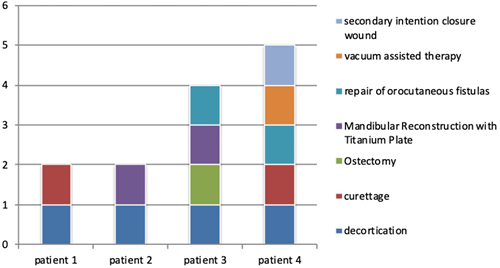
Figure 1. Treatment of the cases with pharmacological ONC
DISCUSSION
In Mexico, there are few or no prospective epidemiological studies that report data in relation to pharmacological ONC. The studies published in relation to osteonecrosis due to drugs, have mostly been retrospective, such as presented by Chaurand et al., from the ISSSTE National Medical Center November 20, Mexico City; where, unlike the present study, those of these authors were carried out in conjunction with various specialties, which is reflected in the large sample of patients compared to our study (24). Studies by Khan, Stopeck, Henry, Bone and Chaurand among other authors (8,23-26) talk about the prevalence of maxillo-mandibular pharmacological osteonecrosis in this study was also higher in relation to bisphosphonate-type medications (mainly intravenous zoledronic acid) reporting 3 out of 9 patients with treatment with this medication, in the literary review reported a lower prevalence (1 %) of osteonecrosis caused by “denosumab” in relation with another. A study carried out by Kim mentioned that the largest number of cases in his sample were women, in this article we found that despite being a small sample, the largest number were also women (28). On the other hand, the complication and sub-diagnosis of osteonecrosis due to drugs may be due to the fact that it is based only on clinical criteria and stages (previously mentioned, such as those of the AAOMS (5,6) or Bedogni et al. (14)); which can be reflected in diagnostic inaccuracies, taking into account that there are other entities that clinically and imaging can be differential diagnoses of osteonecrosis due to drugs (29). One of the recent literary reviews in 2020, carried out by Ayala et. al. (17) refer to three classes of new agents capable of inducing osteonecrosis of the jaw associated with drugs (OMAM), among which the antiangiogenic drugs such as bevacizumab and aflibercept stand out, the second group of drugs are: tyrosine kinase inhibitors (TKIs [tyrosine kinase inhibitors]) (sunitinib, sorafenib, cabozantinib) and the third group they mention are inhibitors of the mammalian target of rapamycin (mTOR [mammalian target of rapamycin]). In the case of our series of cases, the patients presented were taking bisphosphonates and only one denosumab. Another article that mentions the treatment according to the stage and has a similar management to the one we present is by the author Hamadeh (16) who highlights the use of mouthwashes, antibiotics, and debridement and in case of analgesic pain; such patients present improvement and the progression of the disease can generally be contained. This is similar to what was obtained in this study. One measure that can be adopted is the prevention, carrying out a thorough assessment and examination prior to starting antiresorptive therapy (including drugs such as denosumab, bisphosphonates, among others) in order to reduce the incidence of pharmacological ONC.
CONCLUSIONS
It must be taken into account that pharmacological osteonecrosis may be due to various medications and not exclusively in relation to bisphosphonates, with this there will be a better assessment, diagnosis, prevention and management of the patients who present it. It is always necessary to consider risk factors such as: higher incidence reported in different studies in female patients, middle-aged patients who are associated with physiological processes of their age, and a greater propensity for osteoporosis as well as other degenerative bone diseases, patients of both genders with an oncogenic history (breast or prostate cancer), some immunosuppression coupled with ONC, which presents a major problem since it can have an increased susceptibility to infection and/or other complications. Early diagnosis is accompanied by the correlation of the clinic and image, since it must be taken into account that in early stages of ONC there may or may not be bone exposure or orocutaneous fistulas, but by having cabinet studies we can have a broader view of the entity, likewise make aware of the importance in the prevention and application of palliatives in early stages of ONC. In surgical management, in the Maxillofacial area, it is important that the treatment is carried out in a multidisciplinary way and in a medical-surgical set, to provide better care for the patient. Unfortunately, pharmacological osteonecrosis has been under-diagnosed, since there are other osteolytic entities that can be differential diagnoses (such as osteomyelitis, radio-osteonecrosis, among others). This study aims to initiate a protocol for the early diagnosis and management of patients with ONC for drugs at Specialty Hospital, National Medical Center, “Siglo XXI”, IMSS. Since, as mentioned, the literature related to epidemiological studies in the Mexican population focused on pharmacological ONC is scarce, locally without reaching accurate statistical data at the national level, and the approach is important for the general dentist and doctor, since they are the first contact with patients and can thus be prevented or treated at early stages; and with specialists (Maxillofacial Surgeon, Oncologist Surgeon, Medical Oncologist, Endocrinologists, Pain Clinic Doctors, Laboratory Doctors, Radiologist Doctors, among others) should always be jointly to have adequate management without impacting the patient.
ACKNOWLEDGMENT
Maxillofacial Surgery service, laboratory staff, Infectology, operating room and x-rays.
ETHICAL RESPONSIBILITIES
The authors declare that no experiments on humans or animals have been carried out for this investigation. The protocols of the work center on the publication of patient data have been followed. This article does not Patient data appears, so the confidentiality and privacy as well as the anonymity of the participants have been maintained.
CONFLICT OF INTERESTS
Neither the authors nor any member has a financial or interest relationship (currently or in the last 12 months) with any entity producing, marketing, reselling or distributing health care products or services consumed by, or used in, the patients.
FUNDING
We have not received financing nor do we have sponsors to carry out this study.
REFERENCES