DOI: 10.20986/resed.2020.3842/2020
ORIGINAL
CALCIFIC TENDINITIS OF THE SHOULDER: RISK FACTORS AND EFFECTIVENESS OF IONTOPHORESIS WITH ACETIC ACID 5 % PLUS ULTRASOUND: PROSPECTIVE QUASI-EXPERIMENTAL STUDY AT 5 YEARS WITH 138 CASES
TENDINITIS CALCIFICANTE DE HOMBRO: FACTORES DE RIESGO Y EFECTIVIDAD DE LA IONTOFORESIS CON ÁCIDO ACÉTICO 5 % MÁS ULTRASONIDO: ESTUDIO CUASIEXPERIMENTAL PROSPECTIVO A 5 AÑOS CON 138 CASOS
M. E. Fernández Cuadros1
M. J. Albaladejo Florín1
S. Álava Rabasa1
O. S. Pérez Moro1
1Servicio de Medicina Física y Rehabilitación. Hospital Universitario Santa Cristina. Madrid, España
ABSTRACT
Objective: To characterize clinically calcifying tendonitis (CT) and to conduct a prospective quasi-experimental before-and-after study in order to demonstrate the effectiveness of 5 % acetic acid iontophoresis and ultrasound in the treatment of CT.
Material and methods: Prospective, observational, quasi-experimental before-after intervention study to 138 patients who attended to Rehabilitation Department, Santísima Trinidad's General Foundation Hospital, Salamanca, from June-2014 to December-2018.
Outcome Measures: 1) pain: measured by Visual Analogical Scale (VAS); 2) calcification size: in millimetres (mm); 3) functional limitation of shoulder movement (% of patients), all measured at the beginning/end of treatment.
Intervention: iontophoresis with 5 % acetic acid at 4,7mA x 10 minutes and ultrasound 1W/cm2x 5 minutes over calcification.
Results: Mean age 54.6 years (n = 138). Female (73.1 %; n = 101); female to male ratio 3:1. Supraspinatus tendon (94.6 %; n = 124), subscapularis (5.4 %; n=14); left shoulder (55.1 %; n = 76), right shoulder (44.9 %; n = 62). Bilateral 1.4 % (n = 2). Right handed 96.3 % (n = 133); Personal history: smoking (19.5 %; n = 27), diabetes (7.2 %; n = 10); disease time averaged 6.08 months; acute-subacute pain (less than 3 months) 47.1; (n = 65), chronic pain (greater than 3 months) 52.9 % (n = 73). Radiological type: formative 75.3 % (n = 104); resorptive 24.7 % (n = 34). Average number of sessions: 20.5. Treatment complications 2.8 % (n = 4): intolerance/erythema/burn. Occupation: administrative 39.8 % (n = 55), manual jobs 60.2 % (n = 83).
Average initial pain 7.3 points (VAS scale), significantly decreased (p = 0.0000) post treatment to 2.7. Initial average size of calcifications 10.7 mm and significantly decreased (p = 0.0000) post treatment to 3.8 mm. Change of calcification: success/cure rate 55.7 % (n = 77), improvement rate 20.2 % (n = 28); failure rate 23.9 % (n = 33). Functional limitation decreased from 10.8 % of patients to 2.1 %.
Conclusions: CT is common in middle-aged working women. It affects supraspinatus tendon. It is associated with smoking and diabetes. Occupational risk factors include awkward positions and lighting weights. Iontophoresis with 5 % acetic acid and ultrasound is a safe, simple and inexpensive technique, capable to reduce pain and calcification, and recover functional limitation, with a recommended degree of scientific evidence (2B).
Key words: Iontophoresis, calcific tendinitis, pain, shoulder, ultrasound
RESUMEN
Objetivo: Caracterizar clínicamente la tendinitis calcificante (TC) y demostrar la efectividad de la iontoforesis del ácido acético al 5 % y el ultrasonido en el tratamiento de la TC.
Material y métodos: Estudio prospectivo, observacional, cuasiexperimental, tipo antes y después de la intervención, a 138 pacientes que asistieron al Departamento de Rehabilitación, del Hospital de la Fundación General Santísima Trinidad, Salamanca, de junio de 2014 a diciembre del 2018.
Medidas de resultado: 1) dolor: medido por la escala analógica visual (EVA); 2) tamaño de la calcificación: en milímetros (mm), ambos medidos al inicio/final del tratamiento; 3) limitación funcional (en porcentaje de pacientes) pre/post intervención.
Intervención: iontoforesis con ácido acético al 5 % a 4,7 mA x 10 minutos y ultrasonido 1W/cm2/1Hz/5 minutos sobre calcificación.
Resultados: Edad media: 54,6 años (n = 138); mujer (73,1 %; n = 101); proporción mujer/hombre 3: 1; tendón supraespinoso (94,6 %; n = 124); subescapular (5,4 %; n = 14); hombro izquierdo (55,1 %; n = 76), hombro derecho (44,9 %; n = 62); bilateral 1,4 % (n = 2); diestros 96,3 % (n = 133); antecedentes personales: tabaquismo (19,5 %; n = 27), diabetes (7,2 %; n = 10). El tiempo de enfermedad promedio fue de 6,08 meses. Dolor agudo-subagudo (menos de 3 meses) 47,1 %; (n = 65), dolor crónico (más de 3 meses) 52,9 % (n = 73). Tipo radiológico: formativo 75,3 % (n = 104), resortivo 24,7 % (n = 34). Número promedio de sesiones: 20. Complicaciones del tratamiento 2,8 % (n = 4): intolerancia/eritema/quemadura. Ocupación: administrativo 39,8 % (n = 55), trabajos manuales 60,2 % (n = 83). El dolor inicial EVA de 7,3 puntos disminuyó significativamente (p = 0,0000) después del tratamiento a 2,7. El tamaño promedio inicial de las calcificaciones fue de 10,7 mm y disminuyó significativamente (p = 0,0000) después del tratamiento a 3,8 mm. Cambio de calcificación: tasa de éxito/curación 55,7 % (n = 77), tasa de mejora 20,2 % (n = 28); tasa de fracaso del 23,9 % (n = 33). La limitación funcional disminuyó de un 10,8 % a un 2,1 %.
Conclusiones: La TC es común en mujeres trabajadoras de mediana edad. Afecta el tendón supraespinoso. Se asocia con el tabaquismo y la diabetes. Factores de riesgo ocupacional son las posiciones mantenidas y manipulación de cargas.
La iontoforesis con ácido acético al 5 % más ultrasonido es una técnica segura, simple y económica, capaz de reducir el dolor y la calcificación, y mejorar la limitación funcional, con un grado de evidencia científica recomendado (2B).
Palabras clave: Iontoforesis, tendinitis calcificante, dolor, hombro, ultrasonido
Correspondence: Marcos Edgar Fernández Cuadros
marcosefc@hotmail.com
Received: August 31, 2020
Accepted: December 2, 2020
INTRODUCTION
Calcific tendinitis (CT) is a very common condition in the Rehabilitation setting, and a common cause of functional disability and shoulder pain (1). Its origin is the deposit of calcium carbonate or phosphate on a previously healthy tendon (2,3). The pathogenesis is unknown, but fibrosis and necrosis of the tendon are thought to cause degeneration due to crystal deposition (4,5). However, other authors believe that it is not due to a degenerative process, but rather to a cell-mediated process (5,6,7).
Three stages with clinical/histological/radiological correlation that may overlap have been described: precalcification, calcification (with formative and resorptive phase) and postcalcification (with restoration of the normal tendon architecture) (1,2,6).
The clinical picture is variable, there are asymptomatic patients with casual radiological findings, patients with chronic pain and patients with acute painful crises, often in the resorptive phase (8). The diagnosis is clinical (case history plus physical examination) and radiological (radiography and/or ultrasound) (1,8,9). Treatment is initially conservative and depends on the developmental stage (10). Some authors argue that there may be spontaneous resolution of pain and calcification, reducing it in 9.3% of patients at 1 year, in 33% at 3 years and in 27% at 10 years. This implies that there is a very prolonged time of suffering in patients that affects their quality of life, although it is reduced with appropriate treatment (11). Conservative treatment includes NSAIDs, physical therapy, electrotherapy (microwave, short wave, TENS, ultrasound, iontophoresis, interferential therapy and magnetotherapy) (8). Advanced treatment includes shock waves, aspiration lavage, and arthroscopic shoulder surgery (12).
Although there is no consensus regarding the rehabilitation therapy, in a recent experimental study, Fernández-Cuadros et al. have demonstrated the effectiveness of various electrotherapy techniques in reducing pain, although no decrease in calcification on CT was found (8).
Iontophoresis with acetic acid is a classic, inexpensive and safe treatment, and until a few decades ago it was the only one capable of acting on calcification. However, only few clinical trials support its effectiveness (1,3,13,14,15,16).
Shock waves and shoulder arthroscopy are advanced therapeutic options, just as effective as iontophoresis, although much more expensive, painful, and they may involve risks or complications (1).
The objective of the present study has been to clinically characterize CT and to perform an experimental study that provides a good level of evidence supporting decision-making by demonstrating effectiveness of Iontophoresis with 5% acetic acid plus ultrasound in the treatment of CT of the shoulder.
MATERIAL AND METHODS
To achieve the objective, a quasi-experimental before-and-after study without control group was conducted.
Patients
A total of 138 patients (101 women, 37 men) diagnosed with shoulder CT who attended the Clinical Rehabilitation Service of the Fundación Hospital General Santísima Trinidad de Salamanca between June 2014 and December 2018 (54 months) were included.
Inclusion criteria
Exclusion criteria
Assessment
In the first consultation, the sociodemographic data (age, sex, occupation, laterality, dominance), medical hystory (diseases, pacemaker, electrical stimulator), and the radiological type of the calcification (formative or resorptive) are obtained. The articular balance of the shoulder was assessed in its four movements (abduction, antepulsion, internal and external rotations), characterizing it as limited or complete; in addition, functional shoulder tests were applied. These assessments were repeated at the end of treatment.
Outcome variables
Intervention
The treatment consisted of the application of Iontophoresis with 5% acetic acid, 2 cc that were soaked on a gauze and placed on the previously moistened cation (Figure 1), and placed on the anterior face of the affected trochiter. The anion, also moistened, was placed at a distance of 10 cm from the cation, at the posterior edge of the shoulder (on the supraspinatus fossa), to allow the passage of current flow. Both electrodes covered with moistened cloths were fastened with a velcro around the shoulder, allowing full contact on the shoulder and thus avoiding the risk of burns (Figure 2). A galvanic current was applied at an intensity of 4.7 mA for 10 minutes. If the patient did not tolerate this intensity, it was reduced to 2 mA and applied for 20 minutes (Figure 1). Subsequently, continuous ultrasound was applied at an intensity of 1 w/cm2/1 MHz/5 minutes, on the trochiter to promote the absorption of the drug and reduce pain (3).
Fig. 1. Acetic acid 5% (negative polarity) is poured in an amount of 2 cc on a cotton gauze over the cation (negative electrode). For iontophoresis, a galvanic current of 4.7 mA is applied for 10 minutes.

Fig. 2. The cation (negative electrode) is applied on the anterior aspect of the shoulder (anterior image) while the anion (positive electrode) is applied 10 cm away, in the posterior region of the shoulder, on the supraspinatus fossa. Both electrodes are pre-moistened and fastened with a velcro.
Following-up
Periodic check-ups (every 10 days) were performed to assess pain and radiological change in the size and/or disappearance of the calcification. The minimum significant clinical change for pain measured by VAS (Visual Analogue Scale) corresponds to one point; a significant improvement is considered if the change is greater than 3 points (17). The radiological/ultrasound measurements of the calcification were performed in mm, assessing the calcification using its longest axis. If there was more than one calcification, the total measurement corresponded to the sum of the present calcifications measured separately. The effectiveness of treatment with iontophoresis considering the outcome variable “size of calcification” was assessed as follows: 1) cure/success (if the calcification disappeared or decreased more than 75%); 2) improvement (if calcification decreased between 25-75%); 3) failure (if calcification decreased less than 25% or did not decrease). Clinical improvement included decreased pain (measured by VAS), disappearance of painful maneuvers, and recovery of functional mobility (limited or not limited).
SPSS® 20.0 was used for the collection and statistical processing of the variables. Means were used for the qualitative descriptive variables, whereas frequencies and percentages were used for quantitative variables. The Student’s t test was used to compare quantitative variables, whereas the Chi square test was used to compare the qualitative variables. The level of significance used was 99% (p <0.01).
RESULTS
The age of the patients in the sample was 54.6 years (n = 1 38). The most frequent sex was female (73.1%; n = 101), with a 3/1 female/male ratio (Table I). Among the history associated with CT, smoking (19.5%; n = 27) and diabetes (7.2%; n = 10) stood out (Table I).
The most affected tendon was the supraspinatus tendon (94.6%; n = 124), followed by the subscapularis tendon (5.4%; n = 14) (Table I). Regarding laterality, the most frequently affected shoulder was the left one (55.1%; n = 76), followed by the right (44.9%; n = 62). Only two patients had bilateral CT (1.4%; n = 2) (Table I). Regarding dominance, most of the patients were right-handed (96.3%; n = 133).
Table I. Evaluation of the main variables studied (n = 138)
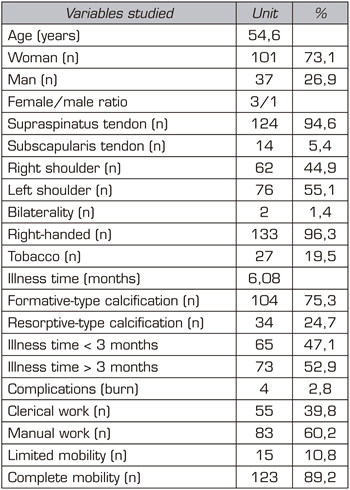
The mean illness time in this study was 6.08 months. Acute-subacute pain (less than 3 months) was less frequent (47.1%; n = 65) than chronic pain (more than 3 months) (52.9%; n = 73) (Table I).
The most frequent radiological type was formative (75.3%; n = 104), followed by resorptive (24.7%; n = 34). The average number of sessions applied was 20.5. A total of 2.8% of the patients (n = 4) stopped the treatment due to intolerance, erythema and/or burn; therefore, they completed the treatment with ultrasound or short wave according to tolerance (for pain management). With regard to occupation, 39.8% (n = 55) were clerical work, while 60.2% (n = 83) conducted a manual work (Table I).
Regarding mobility, 10.8% (n = 15) of the patients presented functional limitation in the affected shoulder (Table I).
The mean initial pain was 7.3 points on the VAS scale, and it decreased significantly (p = 0.0000) after treatment to 2.7 points (Figure 3). The initial mean size of the calcifications was 10.7 mm and it decreased significantly (p = 0.0000) to 3.8 mm after treatment (Figure 3).
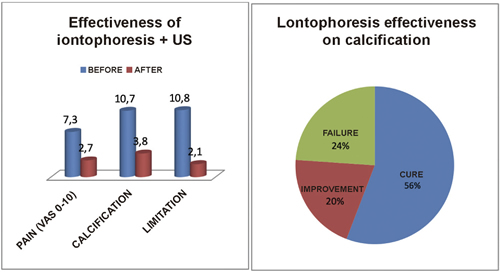
Fig. 3. Effectiveness of iontophoresis on pain (VAS 0-10), calcification size (mm) and functional limitation (%) in patients with calcific tendinitis of the shoulder.
The change in calcification is considered an outcome variable, which considered the disappearance (decrease of more than 75%), decrease (reduction between 25-75%) or no decrease (reduction of less than 25%) of the calcification. This allows us to evaluate treatment as success/cure, improvement, or failure, respectively. This represented a success/cure rate of 55.7% (n = 77), improvement of 20.2% (n = 28), and failure of 23.9% (n = 33) (Figure 3).
After treatment, only 3 patients (2.1%) out of the 15 patients with functional limitation (10.8%) remained with limitation, for which they required manual therapy (20 sessions on average) for their complete recovery (Figure 3).
DISCUSSION
The objective of the present study has been to provide demonstrable clinical evidence supporting the use of iontophoresis with acetic acid plus ultrasound in CT, given the scarcity of studies in this regard despite the widespread use of this technique in Rehabilitation Services, its effectiveness and its few adverse effects.
In fact, the use of acetic acid iontophoresis in the treatment of CT of the shoulder has been the most frequently applied therapeutic modality in rehabilitation services for decades. However, only few studies supporting its use (3,16) are available; some of them show inconsistent results (14,15). This is the first study supporting the use of acetic acid iontophoresis plus ultrasound with demonstrable scientific evidence and with a case series (n = 138) higher than that of previous studies (11, 18 and 34 patients, respectively) (3, 14,15) and in a 5-year prospective study.
CT is a frequent, painful and disabling disease producing a large socioeconomic impact (18), a large demand and use of resources (19) and work absenteeism (8).
Pain is the leading cause of disability due to loss of mobility. In this study, 10.8% of the patients (n = 15) presented mobility limitation. This has a great impact on the quality of life. Some authors maintain that these pains remain in 50% of cases up to a year after the first consultation (19), while others state that CT can spontaneously evolve towards cured after 3 to 10 years (11), which has a negative impact on patients’ quality of life, affecting their personal, family and work spheres (8).
CT is frequent in working patients, with a mean age between 30 and 50 years, as stated by most authors (8,16,18). The mean age in our study was 54.6 years. It is consistent with the reported by Chico-Álvarez (52.5 years) (1), Fernández-Cuadros (53.96 years) (8), Esparza-Ferrera (54 years) (20) and Martínez-Rodríguez (53.1 years) (21); but it is inconsistent with the published by Rioja-Toro (48 years) (3) and by Palma and Kruper (45.2 years) (22).
CT is more common in women, as shown by various studies (2,8,18,20,21), including the present study. The woman/man ratio was 3/1. However, Jacobelli maintains that CT is equally frequent in both sexes (8), while Hernández-Díaz (16) and Hsu (23) describe a larger predominance in males.
The chronic pathology of the rotator cuff and CT is associated with jobs that should be performed in forced postures, lifting weights and performing repetitive movements. Fernández-Cuadros reported that the most frequent occupation in CT was housewife, and for the first time reported an association between CT and occupational risk (8). This is consistent with our results, where 60.2% of the patients are manual workers (they lifted weight) and 39.8% are clerical workers (sustained positions). However, a recent study found that 34.7% of their series were manual workers (they lifted weights) and 65.3% were clerical workers (sustained position) (1).
Most studies show that CT affects the right shoulder (1,3,8,21,24), although up to 25 to 30% may be bilateral (9,18,24). In this study, there was slightly more involvement in the left shoulder (55.1%; n = 76), than in the right shoulder (44.9%, n = 62). Bilateral involvement has also been reported in 1.4% (n = 2), although most of the patients (96.3%, n = 133) were right-handed.
CT most frequently affects the supraspinatus tendon, followed by the infraspinatus and the subscapularis tendons (1,8,20,24,25). In our series, it mainly affected the supraspinatus (94.9%, n = 124), and to a lesser extent the subscapularis (5.1%, n = 14). Similar published studies refer to the supraspinatus in 92% and the subscapularis in 8% (8) and other authors refer to the supraspinatus 80%, infraspinatus 15% and the subscapularis 5% (25).
Radiological diagnosis was performed by using radiography or ultrasound. Magnetic resonance imaging is only indicated in cases of suspected association with soft tissue pathology (8). There are three identifiable stages (clinical/histological/radiological). Uthoff considers the evolutionary stages in: 1) precalcification: tenocyte metaplasia and transformation to chondrocytes; 2) calcification: a) formative (deposition of vesicles in matrix), b) resorptive (spontaneous resorption by macrophages/multinucleated cells by phagocytosis); and 3) Postcalcification: collagen remodeling and tendon repair (1). The various radiological classifications agree that type I corresponds to localized deposits, with well-defined edges, dense consistency and homogeneous texture; while type II corresponds to scattered deposits, poorly defined edges, cloudy consistency and heterogeneous texture (1). This radiological characterization is important, because it is believed that type II (resorptive) has a better prognosis than type I (formative) (8).
Treatment of CT is currently controversial. Recently, Fernández-Cuadros et al. have shown the effectiveness of different rehabilitation techniques (kinesitherapy, short wave, ultrasound, TENS, microwave, interferential therapy) in reducing pain without affecting calcification (8). Until a few decades ago, the only treatment used in the treatment of calcification was iontophoresis with acetic acid. However, there are only three classic articles that assess its effectiveness; one favorably (3) and two unfavorably (14,15). A recent doctoral thesis study performed by Dra. Chico-Álvarez also favorably endorses the use of iontophoresis in CT (1).
Iontophoresis is a non-invasive technique that increases the transdermal penetration of substances (drugs) through the layers of the skin (epidermis, dermis and hypodermis) in a controlled manner and with the help of the application of continuous electrical current, based on the physicochemical principles of attraction and repulsion of charges (26). Its most common applications are: 1) calcific tendinitis and myositis ossificans (acetic acid) (27); 2) control of muscle spasms (calcium chloride and magnesium sulfate); 3) inflammation (dexamethasone); 4) soft tissue inflammation (lidocaine); 5) acute joint pain in rheumatoid arthritis (zinc oxide) (26). This technique is inexpensive due to the use of inexpensive topical medications and because electrotherapy devices configured for the application of iontophoresis has decreased in size and become more accessible due to low production costs (28).
The application of ultrasound to the skin increases its permeability and facilitates the diffusion of different substances to and within the skin. This transport is called sonophoresis (29). Low-frequency sonopheresis works synergistically with iontophoresis, as demonstrated by Le et al. Dr. Le used ultrasound for 10 minutes prior to the application of iontophoresis (30).
In 1955, Psaki and Carrol introduced acetic acid iontophoresis as an effective treatment for shoulder CT (14,15,31). Kahn considers that insoluble calcium carbonate precipitates could be transformed into soluble calcium acetate salts, which would favor the reabsorption of calcification (31): Ca CO3 + 2H(CaH302)2 = Ca(C2H3O2)2 + H20 + CO2.
In addition, the use of ultrasound for its mechanical and thermal effects could help disintegrate and reabsorb calcium deposits by increasing local vascularization (3).
The protocol of our study consisted of the application of iontophoresis with 2 cc of 5% acetic acid, 4.7 mAx 10 minutes, followed by continuous US 1 w/1 Hz/cm 2 x 5 minutes. This protocol differs from that of Rioja-Toro (3), who applied iontophoresis with 3 cc of 5% acetic acid at 4.7 mA for 20 minutes plus 1.5 W/cm 2 ultrasound. Perrón used iontophoresis with 5% acetic acid (no amount specified) at 5 mA x 20 minutes followed by ultrasound 0.8 W/cm 2 x 5 minutes (14). Leduc performed iontophoresis with 2 cc of 5% acetic acid at 5 mA x 15-20 minutes without ultrasound (15). Chico-Álvarez applied iontophoresis with 5% acetic acid (no amount specified) at 4.7 mA for 20 minutes without ultrasound (1).
The average number of sessions in our series was 20. The criteria for continuing or stopping treatment was the radiological and clinical evolution (Figures 4 and 5). The interventions were performed up to a maximum of 40 sessions. Perrón treated patients for 9 sessions (3 weekly sessions for 3 weeks) (14). Leduc treated with 10 sessions (3 per week for the first two weeks; then one weekly for 4 weeks) (15). Rioja-Toro treated patients for 40 sessions (5 times per week) and evaluated them at 20 and 40 sessions (3). Chico-Álvarez treated patients between 15 and 30 sessions depending on the radiological evolution (5 times per week) (1).
The study that has been performed is a quasi-experimental before-and-after type, and included 138 patients. Perrón (14) conducted a randomized experimental study (n = 11 experimental group; n = 10 control group), the same as Leduc (15) (n = 17 experimental group; n = 10 control group). Rioja-Toro (3) conducted an experimental before-and-after study in 34 patients (n = 34). Chico-Álvarez (1) conducted a randomized experimental study (n = 25 experimental group 1; n = 25 experimental group 2; n = 25 experimental group 3).
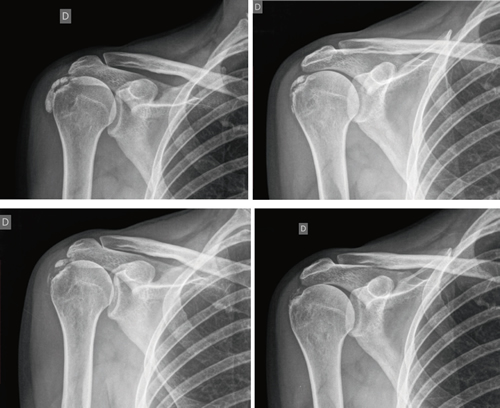
Fig. 4. 47-year-old female patient with formative right supraspinatus calcific tendinitis who, after 30 sessions of iontophoresis, decreased pain measured by VAS from 6/10 to 3/10 and calcification from 38 mm to 8 mm (assessments at onse and at 10, 20 and 30 sessions, respectively).
Our study presented the largest number of patients compared to the studies published to date. The importance lies in the difficulty of prospectively collecting such a number of patients. Perrón (14) collected 21 patients in 4 years (1990-1994); Leduc (15) needed 3 years (1998-2001) for 36 patients, of whom they could only use 27. Rioja-Toro (3) recruited 34 patients in 2 years (1998-2000); and Chico-Álvarez (1) requiered 1 year to recruit 25 patients for each control group (2013). We recruited 138 patients in a 5-year prospective study (July 2014 to December 2018).

Fig. 5. A 44-year-old female patient, with calcific tendinitis of the left supraspinatus, of the resorptive type, who after 20 sessions of iontophoresis decreased pain measured by VAS from 10/10 to 4/10, and calcification from 22 mm to 0 mm (complete disappearance).
With the protocol of this study we have achieved a significant decrease in pain from 7.3 to 2.7 points on the VAS pain scale. This finding is similar to that of Chico-Álvarez (1), who decreased pain from 5.7 to 2.7. Perrón (14) and Leduc (15) achieved pain improvements, although not significant. Rioja-Toro (3) reported disappearance of pain in 54% and improvement in 25% of their series, this is a cure-improvement of 79.6%. Hernández-Díaz (16) found an improvement in moderate-severe pain (95.6%) at the onset to mild-no pain (95.7%) at end (16) after 10 sesions of iontophoresis with 2% acetic acid. All studies, including ours, show that iontophoresis with acetic acid reduces pain on shoulder CT.
Our treatment protocol (iontophoresis with 5% acetic acid plus ultrasound) is capable of significantly reducing the size of the calcification on average from 10.7 mm (onset) to 3.8 mm (end). We have found a success rate (75-100% disappearance of calcification) of 55.7% (n = 77), an improvement rate (25-75% decrease of calcification) of 20.2% (n = 28), and a failure rate (decrease less than 25%) of 23.9% (n = 33). This result is consistent with the described by Rioja-Toro, who reported a 13.2% disappearance of calcification and a 46.4% decrease; that is a 59.6% modification of the calcium deposits (3). Hernández-Díaz reported a success rate of 43.5%, an improvement rate of 52.2%, and a failure rate of 4.3% (16). Chico-Álvarez observed a radiological decrease in calcification from 9.1 mm (onset) to 5.7 mm (at the end of treatment), and 3.4 mm at 6 months of follow-up. In our series, the rapid decrease in calcification is probably because ultrasound favors the absorption of acetic acid and the dissolution of calcifications. Perrón and Leduc obtained radiological improvement in calcium deposits after treatment with iontophoresis, although with no difference compared to the control. This difference is probably due to the lower number of sessions performed (9 and 10, respectively).
In our series, after the applied treatment, only 2.1% out of 10.8% presenting functional limitation (n = 15) remained with shoulder stiffness (n = 3), thus requiring manual therapy later. Although it was not the objective of this study, we should mention that after 20 sessions of manual therapy (on average), all patients regained their mobility (n = 3). With this in mind, we have recently proposed in a review article, a treatment algorithm for shoulder CT, in which we suggest that patients with functional limitation should undergo manual therapy (kinesitherapy) (32). In addition, patients with pain can improve these symptoms with different rehabilitation techniques (electrotherapy, thermotherapy, etc.). Whereas, for the definitive resolution of calcification, iontophoresis with acetic acid constitutes a first-line non-invasive rehabilitation modality (32). Second-line treatments include shock waves. In case of failure of the previous therapies, the most invasive measures include ultrasound-guided aspiration lavage and arthroscopic surgery (32). Figure 6.
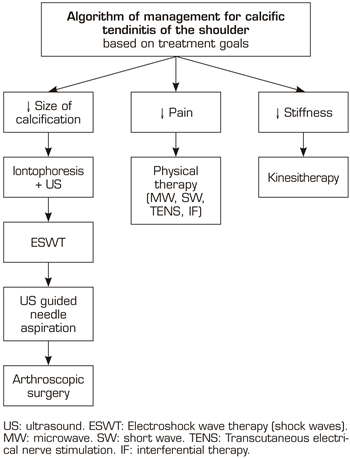
Fig. 6. Algorithm of management for calcific tendinitis of the shoulder based on treatment goals (authorized by Fernandez-Cuadros et al.) (32).
As a contribution to this study, it should be noted that it is difficult to conduct prospective studies capable of collecting sample size like the one that has been studied in the present study. We urge researchers to reproduce studies like ours in order to increase the consistency and evidence of the results observed in this clinical research.
As adverse effects, 2.8% patients (n = 4) presented intolerance, erythema or burn, for whom iontophoresis was stopped. However, these patients completed their sessions only with ultrasound, due to its analgesic properties, reducing pain after treatment, with no decrease in calcification.
CONCLUSIONS
CT is more common in middle-aged working women. The supraspinatus tendon is affected more frequently. It is associated with smoking, diabetes, and jobs that handle loads or perform repetitive maneuvers.
Iontophoresis with 5% acetic acid plus ultrasound is a safe, simple and inexpensive technique, capable of reducing pain and calcification, and recovering mobility in shoulder CT.
The present study shows a 2B level of evidence and grade B recommendation that allows to postulate iontophoresis with acetic acid plus ultrasound as an effective technique, with a recommended level of scientific evidence.
REFERENCES