DOI: 10.20986/resed.2020.3744/2019
ORIGINAL
Symptomatic treatment for migraine. Drugs used and related variables. Results of the european survey on work and migraine
Tratamiento sintomático en migraña. Fármacos utilizados y variables relacionadas. Resultados de la encuesta europea sobre trabajo y migraña
M. T. Vicente-Herrero1
M. V. Ramírez Iñiguez de la Torre1
E. Ruiz de la Torre2
L. Reinoso Barbero3
1Grupo de Trabajo de Guías y Protocolos Asociación Española de Especialistas en Medicina del Trabajo. España
2Presidenta de la European Migraine and Headache Alliance. España
3Presidente de la Asociación Española de Especialistas en Medicina del Trabajo. España
ABSTRACT
Goals: To know the use of migraine crisis symptomatic treatments in different countries of Europe and the differences observed depending on social and demographic variables.
Material and methods: Cross-sectional observational study by anonymous web survey to 3,342 patients from Spain, Italy, France, Portugal, Ireland, United Kingdom, Germany and other countries of the European Union. Study variables: age, gender, country, type of location, level of studies and rural or urban area. The symptomatic treatments that are collected are: simple analgesics, non-steroidal anti-inflammatory drugs, triptans, other treatments, several treatments, without treatment, ignorance of symptomatic treatment.
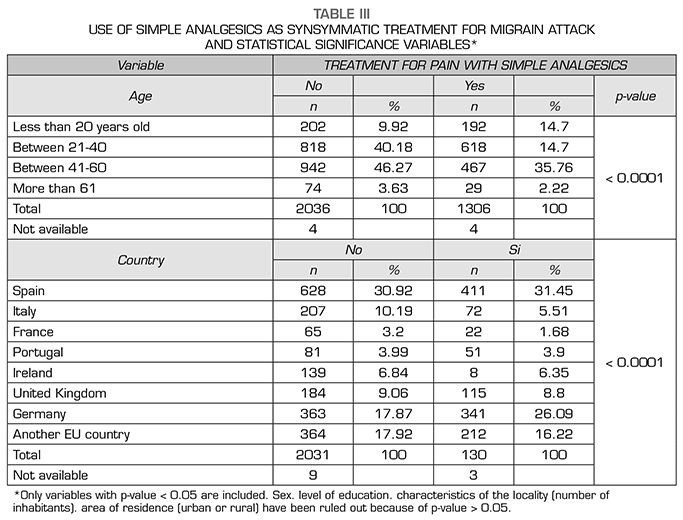
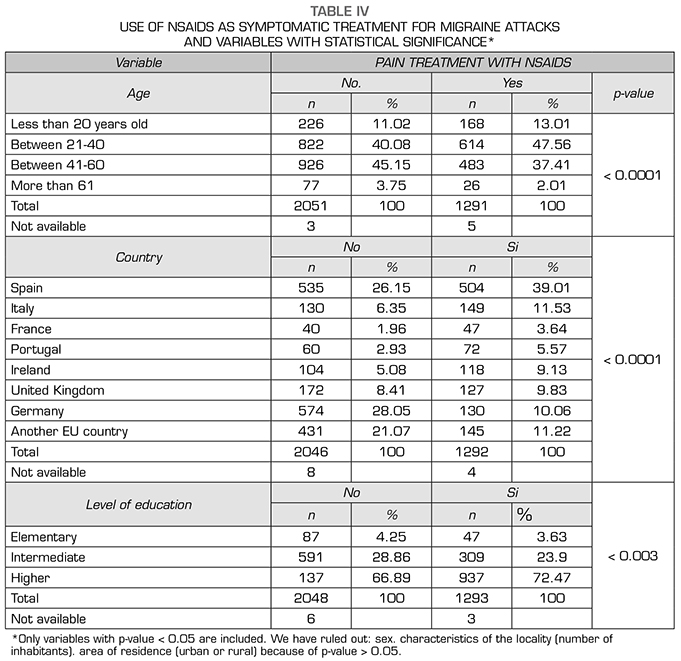
Results: For simple analgesics, the largest consumers are between 41-60 years (p < 0.0001). Spain and Germany are the countries with the highest use (p < 0.0001). For the anti-inflammatories, the greatest use is between 21-60 years (p < 0.0001). Spain, Italy and Germany are the countries that make the most use of them (p < 0.0001) and higher consumption in patients with higher education (p < 0.003).
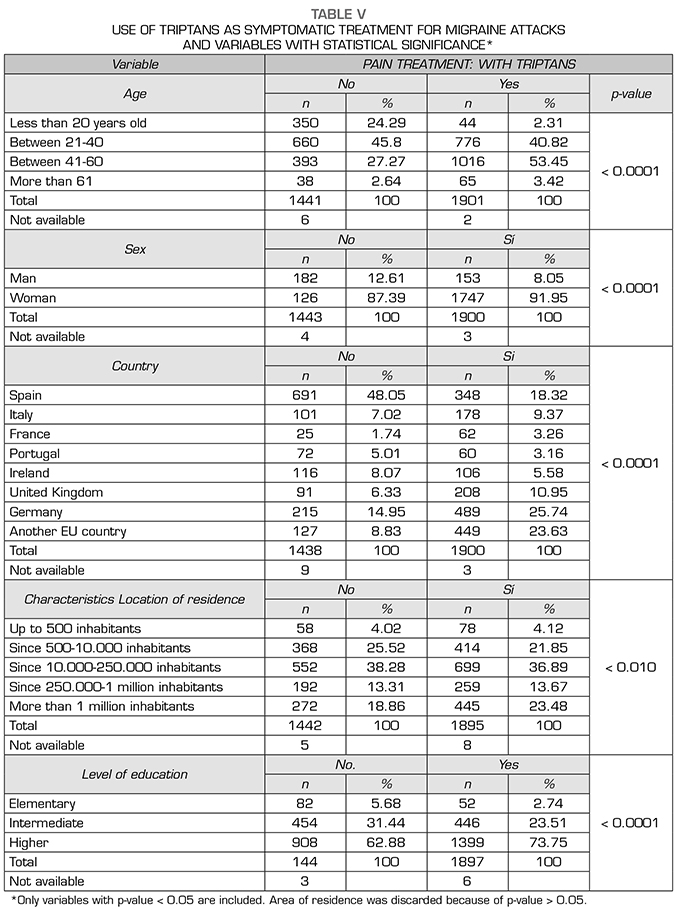
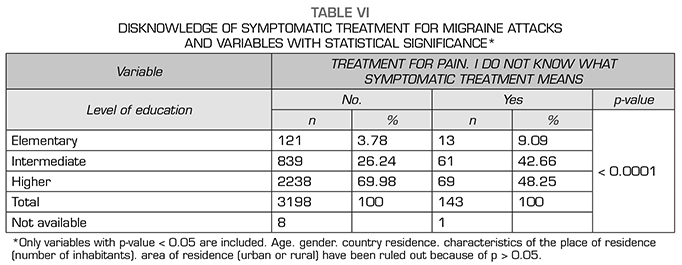
Triptans use shows a relationship with age and gender, greater use between 21-60 years (p < 0.0001) and in women (p < 0.0001). By countries, the highest consumption is in Germany, the rest of the European Union countries, Spain and the United Kingdom (p < 0.0001). Greater consumption in patients living in cities with more than 500 inhabitants (p < 0.010) and with medium or higher studies (p < 0.0001). In the group of middle and upper studies, we find, by contrast, the highest percentage of patients who do not know what a symptomatic treatment is (p < 0.0001).
Conclusions: The result varies according each country greatly and they are modified depending on different social and demographic conditions, being the age, gender, rural or urban environment and cultural level the factors that most affect the use of each symptomatic medication for the migraine crisis.
Key words: Migraine, symptomatic treatment, pain, occupational medicine, occupational health, survey
RESUMEN
Objetivos: Conocer el uso de tratamientos sintomáticos para las crisis de migraña en distintos países de Europa y las diferencias que se observan en función de variables sociales y demográficas.
Material y métodos: Estudio observacional transversal mediante encuesta anónima vía web a 3342 pacientes de España, Italia, Francia, Portugal, Irlanda, Reino Unido, Alemania y otros países de la Unión Europea. Variables de estudio: edad género, país, tipo de localidad, nivel de estudios y ámbito rural o urbano. Los tratamientos sintomáticos que se recogen son: analgésicos simples, antinflamatorios no esteroideos, trip-tanes, otros tratamientos, varios tratamientos, sin trata-miento, desconocimiento de tratamiento sintomático.
Resultados: En analgésicos simples los mayores consumidores están entre 41-60 años (p < 0,0001). España y Alemania son los países con mayor uso (p < 0,0001). El cuanto a los antinflamatorios el mayor uso se da entre 21-60 años (p < 0,0001). España, Italia y Alemania son los países que mayor uso hacen de ellos (p < 0,0001) y mayor consumo en pacientes con estudios superiores (p < 0,003).
El uso de triptanes muestra relación con la edad y el género, mayor uso entre 21-60 años (p < 0,0001) y en mujeres (p < 0,0001). Por países, el mayor consumo es en Alemania, resto de países de Unión Europea, España y Reino Unido (p < 0,0001). Mayor consumo en pacientes que viven en ciudades de más de 500 habitantes (p < 0,010) y con estudios medios o superiores (p < 0,0001). En el grupo de estudios medios y superiores se encuentra por contraste el mayor porcentaje de pacientes que desconocen qué es un tratamiento sintomático (p < 0,0001).
Conclusiones: Existe una gran variabilidad de los resultados en cada país y se modifican en función de distintas condiciones sociales y demográficas, siendo la edad, el género, el ámbito rural o urbano y el nivel cultural los factores que más condicionan el uso de cada medicación sintomática para las crisis de migraña.
Palabras clave: Migraña, tratamiento sintomático, dolor, medicina del trabajo, salud laboral, encuesta
Correspondence: M.ª Teófila Vicente-Herrero
mtvh@ono.com/grupo.gimt@gmail.com
Received: 15-05-2019
Accepted: 15-05-2020
INTRODUCTION
Migraine is a disease with a high global prevalence and disabling. and it is accepted that it is not properly diagnosed or treated. This is shown by the results of the EUROLIGHT study performed in 10 European countries (Germany. Italy. Lithuania. Luxembourg. the Netherlands. Spain. Austria. France. the United Kingdom and Ireland) with 9247 patients participating. This study shows that very few people with migraine in rich European countries visit the doctor and migraine-specific drugs are used inappropriately. even among those visiting the doctor. which suggests that there is a need to improve the care of people with headaches and the training aspects of health care managers and patients (1).
The study “My Migraine Voice”. conducted in 31 countries in North and South America. Europe. the Middle East and North Africa. and the Asia and Pacific region. is also in this line. A total of 11266 people were involved in this study and it aimed at understanding the total burden and impact of the disease when attacks last more than 4 days per month. The results of this study suggest that correctly indicated and used treatments and future development advances would address current needs and allow people with migraine to maximize their contribution to society (2).
In Europe. the social and economic impact of migraine is related to the duration of attacks and its inadequate control. which has an impact on quality of life. loss of work productivity and the high use of health resources (3). In addition. many migraine patients do not visit a doctor. or do not achieve adequate relief after consultation as a result of inappropriate or inadequate treatment. and there is still an unmet need for migraine care (4).
The aim of the present study is to know the use of symptomatic treatments for migraine attacks in different European countries and the differences found in terms of different social and demographic conditions. in order to be able to propose more effective and targeted actions in the future based on the results obtained.
MATERIAL AND METHODS
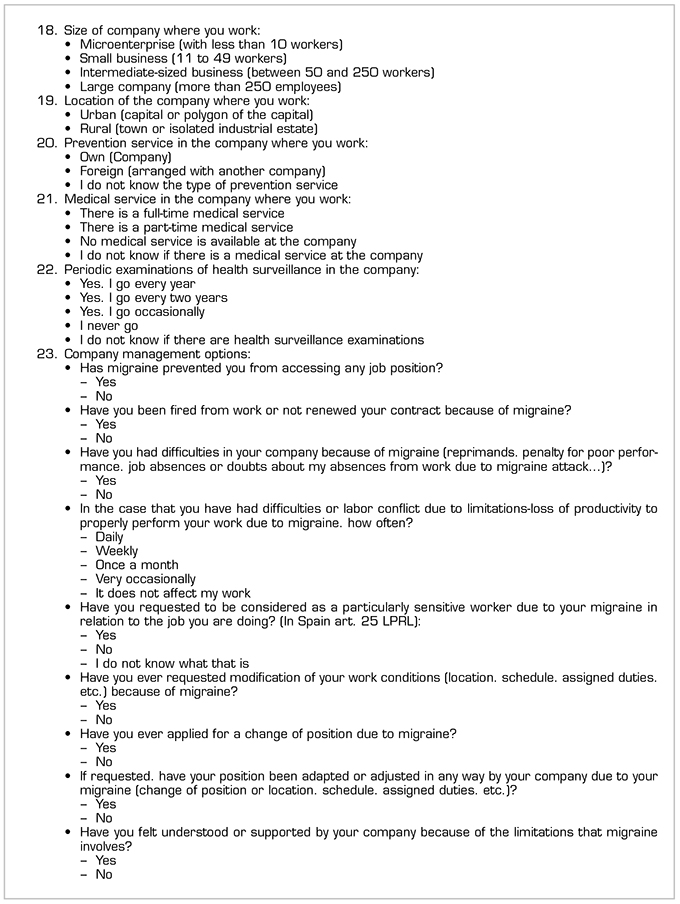
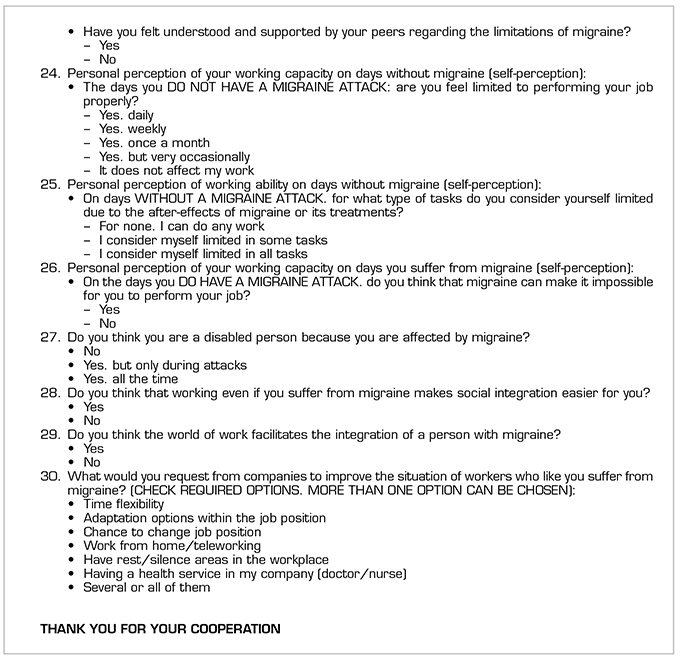
A cross-sectional observational study based on an anonymous web-based survey located on the European Migraine and Headache Alliance (EMHA) website and scientifically endorsed by the Spanish Association of Specialists in Occupational Medicine (AEEMT) to 3342 patients in Spain. Italy. France. Portugal. Ireland. United Kingdom. Germany and other countries of the European Union. A previous diagnosis of migraine. be working at the time of the survey or have been working in the previous year. and participate voluntarily were considered inclusion criteria. Data were collected from September 2018 to January 2019. The survey consists of 32 questions with multiple responses (Annex 1).
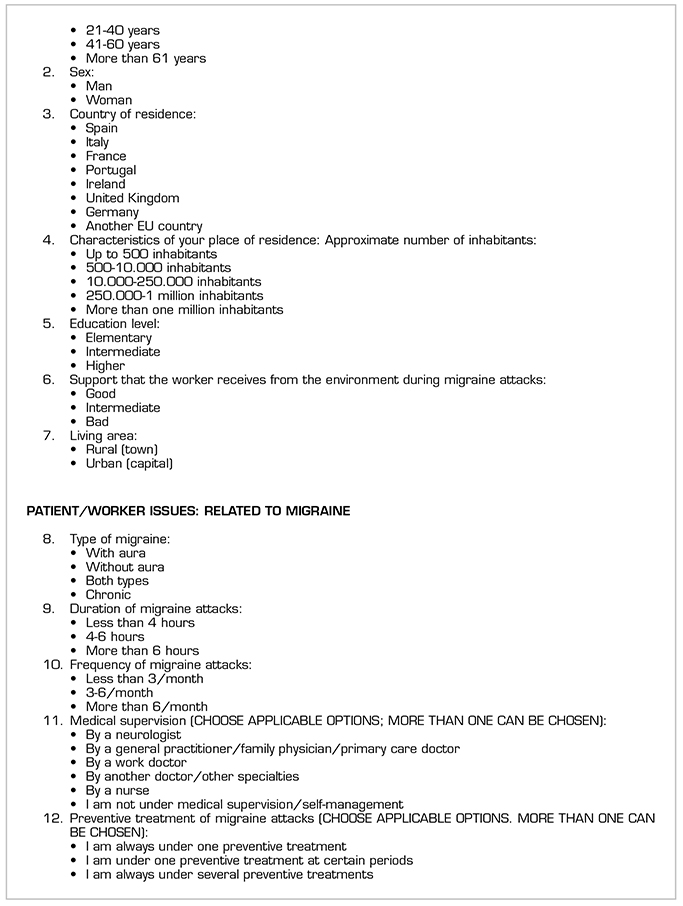
Based on the initial description. the symptomatic treatments used for the treatment of attacks are specifically analyzed according to a series of sociodemographic variables: Age (less than 20 years. between 21 and 40 years. between 41 and 60 years. more than 61 years). sex (male. female). place of residence (Spain. Italy. France. Portugal. Ireland. United Kingdom. Germany. another EU country). type of locality where they reside (up to 500 inhabitants. 500-10.000 inhabitants. 10.000-250.000 inhabitants. 250.000-1 million inhabitants. more than 1 million inhabitants). level of education (elementary. intermediate. higher). area in which they live (rural [town]. urban [capital]).
The symptomatic treatments used are defined by question 13 of the questionnaire (Treatment for pain when you have migraine attacks: With simple analgesics. with nonsteroidal anti-inflammatory drugs (NSAIDs). with triptans. with other symptomatic treatments. with several symptomatic treatments not listed above. I am not taking symptomatic treatment. I do not know what symptomatic treatment means).
A bivariate analysis has been performed for each of the types of symptomatic treatments used according to each of the sociodemographic parameters.
Contingency tables showing absolute frequency (N) and percentage (%) for each variable combination are presented. According to the nature of the questionnaire variables (categorical variables). Chi-square test or Fisher’s exact test have been used to analyze the possible relationship between migraine characteristics and sociodemographic variables.
Since question 13 has multiple responses. the data analysis has been performed independently for each of the possible answers.
RESULTS
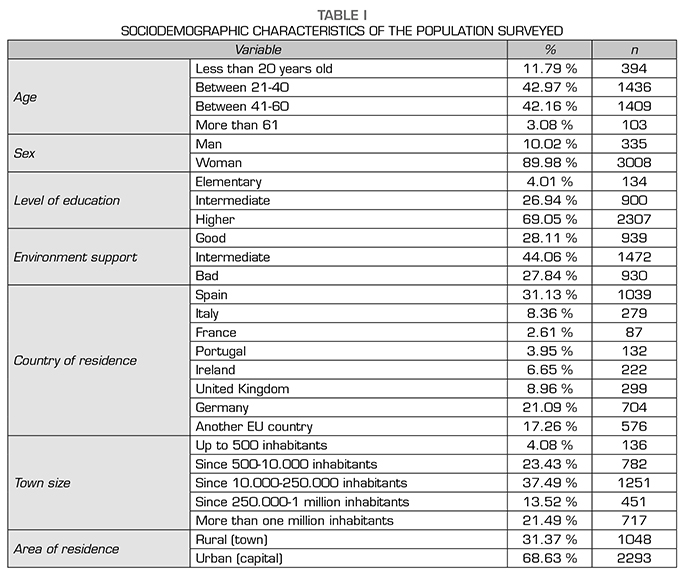
The sociodemographic characteristics of the population that responded to the survey are shown in Table 1 and indicate a heterogeneous distribution by country. with the highest percentage of responses corresponding to Spain and Germany. A total of 85.13% of respondents are in the middle age group and are mostly women (90%). The participants reside mainly in urban areas (68.63 %). in intermediate-large cities (35 % in localities of more than 250.000 inhabitants and 72.5 % in localities of more than 10.000 inhabitants). are skilled workers (69% with higher education and 27% with intermediate studies) and receive moderate support from their environment during migraine attacks (44.06%).
The overall results of the use of the different symptomatic treatments in migraine attacks and their percentage relation with the different sociodemographic variables studied are shown in Table 2.
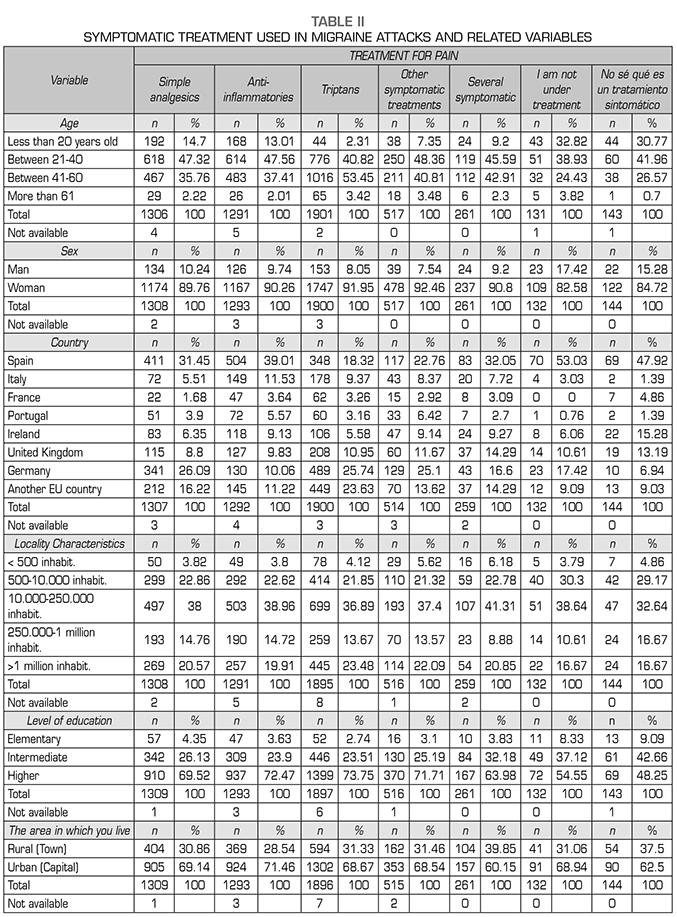
When each of the types of symptomatic treatments are differentiated in relation to the variables studied. and considering only those results with statistical significance we found that:
DISCUSSION
Recommendations for diagnostic criteria and migraine management are regularly updated by the International Headache Society (IHS). the most recent was in 2018 (5). On this basis. the Spanish society of neurology (6) specifies that the suppressive treatment of migraine attacks is indicated for all patients and that it should be personalized. In general. two groups of treatments for attacks are found: Non-specific therapies (simple analgesics and NSAIDs) and specific therapies (triptans-agonists of the 5HT receptors- and ergotic).
Oral NSAIDs are the drugs indicated in mild to moderate attacks (level of evidence I. grade of recommendation A) and. when no response is obtained with these drugs. the recommendation is triptans (level of evidence II. III. and grade of recommendation C).
In severe attacks. the treatment indicated is triptans (grade of recommendation A).
While the criteria seem clear. our survey shows very variable results. We consider simple analgesics. NSAIDs. triptans. and other drugs or drug combinations as treatment options in the survey. The results reveal statistical significance in relation to age. so younger patients use more simple analgesics and/or NSAIDs. whereas patients with ages of 41-60 years use more triptans.
Regarding patients over 60 years. it should be taken into account that migraine especially affects the age group between 21 and 60 years. being less common among those over this age in those who. moreover. the clinical characteristics of migraine are less typical. which makes it difficult to diagnose and treat and involves specific risk considerations due to multi-drug therapy or multi-pathologies that should be assessed (7). The results of our study show that this age group is the group that uses analgesics. NSAIDs and triptans the least.
The results related to the use of pain killers and their sex differences show only statistical significance in the use of triptans. which is larger in women than in men.
This trend on the larger use of triptans in women appears to be consistent in other studies. In 2014. results were published in Piedmont. Italy. on patterns of drug use and administration in patients seeking assistance from pharmacists to alleviate a migraine attack. All epidemiological studies on migraine have consistently shown that it is much more common among women than among men. This gender difference is also reflected in the higher percentage of women receiving treatment or advice for headache attacks. Among the drugs usually taken to relieve headache. there were no statistically significant differences between men and women in the usual use of NSAIDs. in consistency with the results obtained in our study. Statistically significant differences arose in the use of triptans and the use of combination drugs. but not in the use of simple analgesics (8).
Our survey shows differences by country in the use of pain treatments. Spain and the United Kingdom are the least users of treatment and. together with France and Ireland. they are the most unaware of symptomatic treatment. Ireland. United Kingdom and Germany are the countries that use most other treatments. with triptans being the most widely used in all countries except Spain. Portugal and Ireland. NSAIDs are used in all countries participating in the survey. except in Germany and in the group of other countries in the European Union. and simple analgesics are the first choice in Spain and Germany. The results are consistent with the Eurolight study. although this study did not include the differentiation by pharmacological groups that has been performed in our study.
In our study. the use of symptomatic treatments is not influenced by the number of inhabitants of the locality. but the level of education does condition the symptomatic treatment used. being higher the use of NSAID and triptans in people with higher education and. in contrast. lack of knowledge of or use of treatments is prevalent in patients with elementary or intermediate qualifications.
Regardless of the educational level of patients. there seems to be consensus in the scientific community on the advantages of training and information on the disease. Patients consider that having basic information. such as an understandable educational booklet on migraine. means an increase in their general knowledge of the disease and it is useful in increasing attack management (9).
In our study. the area of residence seems to show a trend toward the use of NSAIDs in urban areas and the use of other treatments in rural areas. In most countries. barriers to seeking or accessing health care in rural areas are larger than in urban areas. especially in small areas and those far from urban centers. Literature reviews show imparities in rural and urban health care in countries such as the United States and are oriented toward continuous reform programs aimed at improving the provision of health services. promoting recruitment. training and professional development of health care providers responsible for rural health care. increase comprehensive health insurance coverage. and involve rural residents and health care providers in health promotion (10). This is in line with the observed in countries from very diverse socio-cultural areas and which include aspects linked to deficiencies in access to medical and nursing care (11).
The results of our study reveal a great variability of the results in each country and that they are modified according to different social and demographic conditions. These results are consistent with the suggested by other authors who state that this variability facilitates the evolution toward chronic migraine processes and that all classes of drugs can induce this chronification of the pathology. Drugs that have a higher risk of abuse are among those preferred by patients who are more difficult to treat because of their poor response and a particular impulse toward the consumption of “everything that can be perceived as provider of some relief.” Although these drugs are perceived to be “more potent.” they are often indicated as second- or third-line drugs (12).
The treatment recommendations for migraine attacks are based as a starting point on the correct diagnosis. based on consensus criteria and with personalized therapies according to the conditions of each patient. Several medications are available for the treatment of acute migraine. but not all are effective for all patients. or equally effective in all attacks. Currently. the group of serotonin (5-HT) 1B/1D receptor agonist drugs. called triptans. is the mainstay of acute therapeutic regimens. although there are other approaches to acute treatment. such as simple analgesics. non-steroidal anti-inflammatory drugs (NSAIDs). ergotamines. and combined drugs. Another more recent treatments. in use or under clinical research. are currently assessed (13).
Safety profiles of migraine drugs limit their use in patients with certain comorbid conditions. and adverse effects can also reduce the compliance level of the patient. NSAIDs are often associated with gastrointestinal and possibly cardiovascular side effects. Ergotic alkaloids may induce arterial vasoconstriction. while administration of triptans is contraindicated in cardiovascular. cerebrovascular and peripheral vascular diseases. A number of newly synthesized experimental drugs appear to be effective and promising in the treatment of migraine. but currently experience with them is still limited. and further studies are needed (14).
Today. different types of drugs for acute migraine are discussed. with particular attention to safety problems and possible adverse effects. Although triptans are widely used in the acute treatment of migraine. there is uncertainty about the comparative efficacy of each other and against other specific or used migraine treatments. Triptans used at standard doses are associated with better results than ergotamines and with equal or better results compared to NSAIDs. salicylates. and simple analgesics (15). The frequent use of analgesics. ergotamine alkaloids. and triptans may have an impact on the development of chronic headache due to excessive use of medications. In addition. the onset of a migraine attack is not fully understood. and treatment targeting causal factors is not currently available. The tolerability and adverse effects of currently available drugs limit their use in certain groups of patients. together with the fact that frequent use of these drugs raises the risk of developing adverse effects and. therefore. the need for drugs based on pathological mechanisms within a concept of personalized medicine is imposed (16).
ACKNOWLEDGMENTS
To the patients of the EMHA for their voluntary collaboration in this survey. to the Spanish Association of Specialists in Occupational Medicine for its scientific support and endorsement. and to Silvia Lladosa for the statistical analysis of the data.
CONFLICT OF INTEREST
This study was funded by the European Migraine & Headache Alliance.
REFERENCES