DOI: 10.20986/resed.2021.3922/2021
ORIGINAL
PSYCHOLOGICAL FACTORS ASSOCIATED WITH THE ADHERENCE TO ANALGESIC TREATMENT IN PATIENTS WITH CHRONIC PAIN: SYSTEMATIC REVIEW OF THE LITERATURE
FACTORES PSICOLÓGICOS ASOCIADOS A LA ADHERENCIA AL TRATAMIENTO ANALGÉSICO EN PACIENTES CON DOLOR CRÓNICO: REVISIÓN SISTEMÁTICA DE LA LITERATURA
J. Palomo-Osuna1,2,3
H. De Sola1,2,3
J. A. Moral-Munoz1,2,4
M. Dueñas1,2,5
A. Salaza1,2,5
I. Failde1,2,3
1Instituto de Investigación e Innovación Biomédica de Cádiz (INiBICA). Unidad de Investigación. Hospital Universitario Puerta del Mar. Cádiz, España
2Observatorio del Dolor. Universidad de Cádiz, España
3Área de Medicina Preventiva y Salud Pública. Universidad de Cádiz, España
4Departamento de Enfermería y Fisioterapia. Universidad de Cádiz, España
5Departamento de Estadística e Investigación Operativa. Universidad de Cádiz, España
ABSTRACT
Introduction: The lack of adherence is frequent in chronic pain (CP) patients and the influence of psychological factors may play a relevant role. The aim of this study was to analyze the psychological factors related to the adherence to analgesic treatment in patients with CP.
Methodology: A systematic review was carried out, including original articles published in English and Spanish between June-2009 and June-2019 included in Pudmed, Scopus, Web of Science and PsycINFO. Articles with cross-sectional and longitudinal design were included, carried out in a population >18 years with chronic non-oncological pain (CNOP) and that analyzed any psychological variable in relation to adherence to analgesic treatment. The search terms were “adherence”, “compliance”, “misuse”, “analgesic”, “chronic pain” and “psychology”. The quality of the articles included was analysed through the Critical Appraisal Checklist for Analytical Cross-sectional studies of Joanna Briggs Institute for cross-sectional studies and the Newcastle-Ottawa Quality Assessment Form for Cohort Studies for the longitudinal studies.
Results: A total of 1184 articles were initially identified, and 14 were finally selected. Depression was the most studied variable, being included in 11 articles, followed by anxiety, that appeared in 6. Both depression and anxiety were repeatedly associated with lower adherence to analgesic treatment, and the same was true in two of the articles that measured jointly the relationship of anxiety and depression on analgesic adherence (high negative affect 39.1 % vs. low negative affect 8,3 %, p = 0.013). Active coping strategies were found to be associated with underuse (OR = 1.132, 95 % CI: 1.027-1.249, p = 0.013) and poor coping strategies were associated with opioid misuse (p = 0.01). The association between catastrophizing and analgesic adherence was addressed in 5 articles, and although it was found that catastrophizing was related to low adherence (r = 0.45, p = 0.01), this result was no longer significant when evaluated alongside anxiety and depression.
Conclusion: The identification and control of psychological factors in patients suffering from CP is necessary, as it could serve to improve adherence to analgesic treatment in these patients.
Key words: Chronic pain, systematic review, adherence, psychological factors, analgesic.
RESUMEN
Introducción: La falta de adherencia terapéutica es frecuente en pacientes con dolor crónico (DC) y la influencia de factores psicológicos sobre ella puede ser relevante. El objetivo del estudio es analizar los factores psicológicos relacionados con la adherencia al tratamiento analgésico en paciente con DC.
Metodología: Se realizó una revisión sistemática donde se incluyeron artículos originales publicados en inglés y castellano entre junio de 2009 y junio de 2019 incluidos en Pudmed, Scopus, Web of Science y PsycINFO. Se incluyeron artículos con diseño transversal y longitudinal, llevados a cabo en una población > 18 años con dolor crónico no oncológico (DCNO) y que analizaban cualquier variable psicológica en relación con la adherencia al tratamiento analgésico. Los términos de búsqueda fueron “adherence”, “compliance”, “misuse”, “analgesic”, “chronic pain” y “psychology”. La calidad de los artículos incluidos se analizó mediante la Critical Appraisal Checklist for Analytical Cross-sectional studies de Joanna Briggs Institute para los estudios transversales y Newcastle-Ottawa Quality Assessment Form for Cohort Studies para los longitudinales.
Resultados: Se identificaron 1184 artículos, de los cuales 14 fueron finalmente seleccionados. La depresión fue la variable más estudiada, incluida en 11 artículos, seguida de la ansiedad, que apareció en 6. Tanto la depresión como la ansiedad se asociaron de manera constante y significativa con una menor adherencia al tratamiento analgésico, y lo mismo fue cierto en dos de los artículos que miden conjuntamente la relación de ansiedad y depresión en la adherencia analgésica (efecto negativo alto 39,1 % vs. efecto negativo bajo 8,3 %, p = 0,013). Se encontró que las estrategias de afrontamiento activas se asociaban con infrauso (OR = 1,132, IC 95 %: 1,027-1,249, p = 0,013) y las pobres estrategias de afrontamiento se relacionaron con un mal uso de los opioides (p = 0,01). La asociación entre catastrofismo y adherencia analgésica se abordaba en 5 artículos, y aunque se encontró que el catastrofismo se relacionaba con una baja adherencia (r = 0,45, p < 0,01), este resultado dejó de ser significativo cuando se evaluaba junto a la ansiedad y a la depresión.
Conclusiones: La identificación y control de los factores psicológicos en los enfermos que sufren DC es necesario, ya que podría servir para mejorar la adherencia al tratamiento analgésico en estos pacientes.
Palabras clave: Dolor crónico, revisión sistemática, adherencia, factores psicológicos, analgésicos.
Received: 12-05-2021
Accepted: 18-09-2021
Correspondence: Jenifer Palomo Osuna
jenifer.palomo@uca.es
INTRODUCTION
Chronic pain (CP) is a health problem affecting approximately 19 % of the adult population in Europe (1), and 16.6 % of the population in Spain (2). CP has implications that go beyond the physical distress of the patient, affecting the psychological and social spheres, causing a decrease in quality of life (3-5). In addition, CP has important consequences for work activity because CP has been linked to a decrease in the productivity of working hours (6-8).
Among the interventions recommended to treat CP, those based on a multidisciplinary approach are increasingly used, including non-pharmacological treatments with physical, cognitive-behavioral therapies, exercises, and relaxation therapies, among others (9,10). Despite this, pharmacological treatment is essential for CP control, although the patient’s response to these treatments is often not optimal (11). Some epidemiological studies have shown that between 50 and 70 % of patients with CP take pain relievers to treat pain, and that 4 % use opioids (6,12,13). However, a high percentage of them report severe or unbearable pain (48.9 %) (2).
The lack of adherence to analgesic treatment in patients with chronic non-cancer CP (CNCP) ranges from 8 to 53 %, which could explain, in part, the lack of control of pain reported by the patients (12).
Factors such as being older than 60 years, being a woman, being of a non-Caucasian race, the presence of comorbidities and the high level of stress have been related to the low compliance that a patient with CP has of the analgesic treatment prescribed by his doctor (1,14-16). It has also been shown that the presence of mood disorders and anxiety can condition the low adherence to treatment found in these patients (4). However, the relationship of other psychological factors with treatment adherence in these patients has received little attention, although it seems reasonable to think that they could influence treatment adherence and consequently the response to the treatments of the patients (17,18).
Because of the above, in the present study we aim to identify the psychological factors related to adherence or misuse of analgesic treatment in patients with CNCP through a systematic review of the scientific literature published in recent years.
METHODOLOGY
Design of the study
A systematic review of the literature was conducted according to the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (19). The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with reference number: CRD42020139675.
Search strategy
An exhaustive search of the original articles included in the PubMed, Scopus, Web of Science and PsycINFO databases was performed between June 2009 and June 2019, with a transversal and longitudinal observational design. Articles published in English were included that included patients with CNCP, with a duration of more than 3 months, as defined by the International Association for the Study of Pain (IASP) (20). The keywords and search strategies were: ((((adherence AND analgesic) OR (compliance AND analgesic) OR (misuse AND analgesic) OR “treatment adherence and compliance”[Mesh]) AND “chronic pain” AND “psychology”) AND “last 10 years” [PDat] AND Humans[Mesh]) en PubMed y (TITLE-ABS-KEY (adherence AND analgesic ) OR TITLE-ABS-KEY (compliance AND analgesic) OR TITLE-ABS-KEY (misuse AND analgesic) OR TITLE-ABS-KEY (treatment AND adherence AND compliance) AND TITLE-ABS-KEY (chronic AND pain) AND TITLE-ABS KEY (psychology)) AND PUBYEAR > 2008 AND (LIMIT-TO (LANGUAGE , “English” )) in Scopus y (((adherence AND analgesic) OR (compliance AND analgesic)
OR (misuse AND analgesic) OR (“treatment adherence and compliance”) AND “chronic pain” AND “psychology”)) in Web of Science y PsycINFO.
Eligibility criteria
We included studies performed in a population
> 18 years with CNCP, which aimed to analyze the relationship between the lack of adherence understood as the lack of compliance with the recommendations or prescription provided by the physician (misuse or low adherence to the analgesic treatment) and any psychological variables. Within the studies, it was taken into account that the variables were directly related to the patient and not to the interaction of patients with the physician, family member or their support network. Studies focusing on the abuse of these drugs not including psychological variables, studies based on patients with cancer pain, review articles, meta-analyzes, or short articles were excluded.
Study selection
Two authors reviewed the title and abstract of all articles. Duplicate studies were removed using the Mendeley Desktop 1.19.4 tool. Pre-selected studies were analyzed in depth and also their list of references to identify those that could be included in the present review. The quality of eligible cross-sectional studies was assessed using the Critical Appraisal Checklist for Analytical Cross-sectional studies of Joanna Briggs Institute (21), which includes a checklist containing 8 items. The scores used in the study conducted by Ortega et al. were taken into account for the classification of the included studies. (22), being considered a high-quality article (low risk of bias) when it met at least 5 of the items in this list; studies not meeting this criterion were considered of low quality (Annex 1).
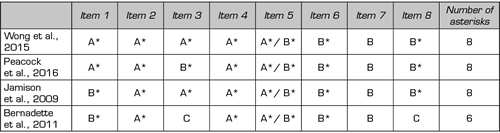
The quality of longitudinal studies was assessed using the Newcastle-Ottawa Quality Assessment Form for Cohort Studies tool (23). This tool evaluates the quality of studies through 8 items grouped into three categories: Selection, comparability, and outcome. Each article can have a maximum of 9 asterisks, and they were considered high quality when they had at least 6 asterisks (22,24) (Annex 1).
RESULTS
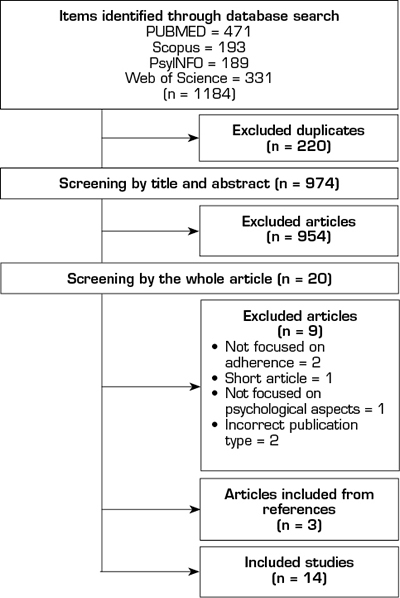
A total of 1184 potential articles were found in the search. After the selection process, 14 articles meeting the inclusion criteria were selected (Figure 1).
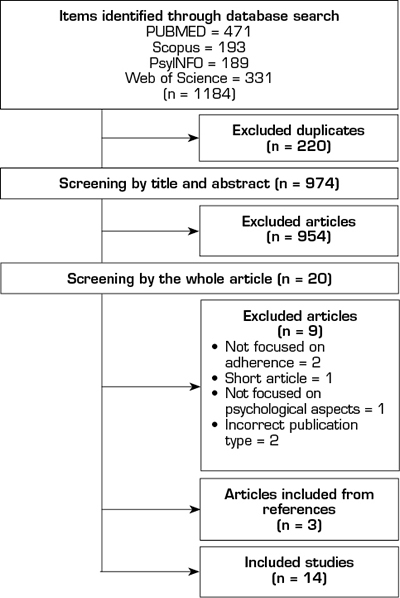
Fig. 1. Flow chart
Quality of studies
All articles included in the review met at least 5 checklist criteria in cross-sectional studies (17,25-33) (Table I) and at least 8 criteria in longitudinal studies (34-37) (Table II), indicating good quality.
Table I. Risk of bias from included cross-sectional studies (n = 10)
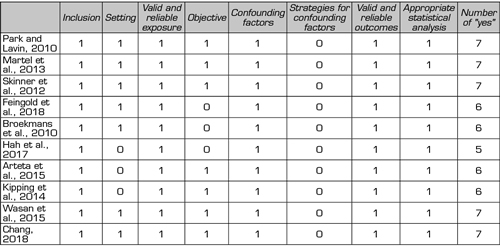
Table II. Assessment of the quality of the included longitudinal studies (n = 4)
General characteristics of the selected studies
Of the 14 studies (Table III), 3 had been conducted in the general population (26,28,33), 7 in patients treated in pain clinics (17,27,30,31,34,36,37), in 3 studies the results came from patients included in health record databases (25,29,35) and in 1 study the patients had been recruited in different health centers or centers for the elderly (32). Of the 14 articles, 4 included patients with CP of specific cause (musculoskeletal pain, spinal pain, chronic low back pain, and headache) (17,33,34,37) and the remainder did not specify the cause of CP. Only 3 of the 13 articles (25,32,33) specified the age group of the population included (Table III) and only 2 articles indicated the response rates which were 57 % and 80.7 % (25,27).
The psychological factors most frequently analyzed in the studies were depression (17,25,27-32,34,36,37), anxiety (27-30,32,35), depression and anxiety measured together (26,33), coping strategies (28,35) and catastrophizing (17,29,30,34,36) (Table III).
Ways to assess adherence, misuse, or low compliance
Adherence, including misuse or low compliance to analgesic treatment, was measured in different ways: Through interviews (28,29,32,35,37), with The Current Opioid Misuse Measure (COMM) (27,30), Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) (17,33,36), Pain Medication Questionnaire (PMQ) (25), urine and blood tests (31), and other assessment tools specified in Table II. Patients were found to be non-adherent, misused, or underuse when they did not take analgesic drugs as prescribed by their physician (Table III).
Relationship between depression and adherence to treatment
The relationship between depression and adherence to analgesic treatment was analyzed in 11 out of the 14 articles (17,25,27-32,34,36,37). Of these, in the 9 using different scales, the presence of depression was found to be related to lower adherence or misuse of these drugs (17,25,27,28,30-32,36,37) (Table III). In one of the previously mentioned studies (27), patients were more likely to abuse opioids among people with moderate depression (adjusted OR = 4; 95 % CI = 1.1-14.58), moderate-severe depression (adjusted OR = 8.56; 95 % CI = 2.19-33.37), and severe depression (adjusted
OR = 23.5; CI 95 % = 5.12-107.81). However, in 2 other studies using the Anxiety and Depression Scale (HADS) and the Patient-Reported Outcomes Measurement Information System (PROMIS) no relationship was found between these two variables (29,34) (Table III).
Table III. Characteristics of the studies included in the systematic review
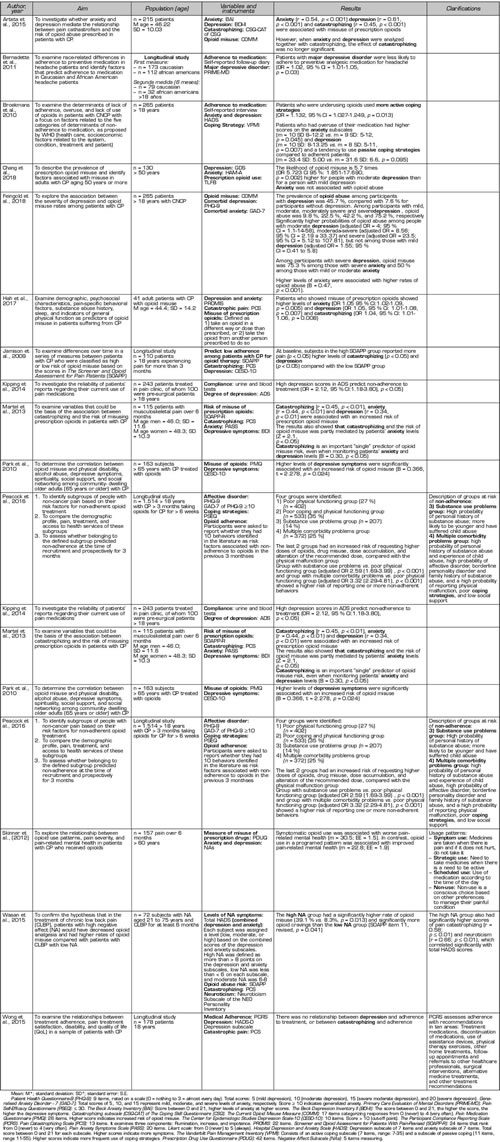
Relationship between anxiety and adherence to treatment
The relationship between anxiety and adherence to treatment was analyzed in 6 articles, and one of them found (30) that a high score on the Beck Anxiety Inventory (BAI) scale, that is, a higher level of anxiety, was associated with low adherence (r = 0.54, p < 0.001).
Furthermore, in a study using Generalized Anxiety Disorder scale (GAD-7) (35), comparing the group with problems due to the use of substances and the group with problems of multiple comorbidity vs. group of poor physical functioning, in both cases they were found to be associated with an increased risk of being non-adherent to opioid therapy (adjusted OR = 2.59, 95 % CI:1.69-3.99, p < 0.001, and adjusted OR = 3.32, 95 % CI:2.29-4.81, p < 0.001, respectively) (Table III). In contrast, two other studies using PROMIS (29) and the Hamilton Anxiety Rating Scale (HAM-A) (32) found no significant relationship between anxiety and opioid misuse.
In the remaining 2 studies, higher scores on the Hospital Depression and Anxiety Scale (HADS) (higher levels of depression and anxiety) were shown to increase the risk of non-adherence (28) when comparing adherent participants versus participants overusing analgesics (anxiety, p = 0.045; depression, p = 0.007). The other study (27) evaluating anxiety using The Generalized Anxiety (GAD-7) showed that as scores on this scale increased (B = 0.47, p < 0.001), opioid misuse increased. In addition, in this study, among patients with severe depression, opioid misuse was 75.3 % in those with severe anxiety and 50 % in those with mild or moderate anxiety (27) (Table III).
Depression and anxiety measured together (negative affect) and adherence to treatment
Two of the articles included in the review measured depression and anxiety together. In one of them (26), it was observed that patients who used opioids only when they felt pain (symptomatic use) had worse mental health than patients who had a pattern of scheduled use of these drugs (they were not taken exactly as directed by their doctor, but it was always taken at the same time: Mean = 30.5; standard error (EE) = 1.5; scheduled use: Mean = 22.8; EE = 1.9). In addition, the other study (33)found that subjects with higher scores in the HADS scale had a higher risk of opioid misuse compared to the group with low score (39.1 vs. 8.3 %, p = 0.013) (Table III).
Relationship between coping strategies and adherence to treatment
The relationship between coping and adherence to analgesics was analyzed in only 2 studies, showing that people with more active coping strategies were at increased risk of non-adherence to analgesics due to underuse (OR = 1.132, 95 % CI: 1.027-1.249, p = 0.013). However, patients with a more passive coping strategy tended to show a lack of adherence due to drug overuse compared with patients with adherent behaviors (mean = 33.4 standard deviation (SD): 5.00 vs. mean = 31.6 SD: 6.6, p = 0.095) (28). Although evaluated on a different scale, another study (35) also found that patients with poor coping strategies were more likely to be non-adherent (Table III). It was also shown that these patients were highly likely to have a borderline personality disorder and little social support (35).
Relationship between catastrophizing and adherence to treatment
We identified 5 studies analyzing the relationship between catastrophizing and adherence to analgesic treatment. In 3 of them, it was found that when the levels of catastrophizing measured with The Pain Catastrophizing Scale (PCS) were high, the risk of non-adherence or misuse of opioids was higher (17,29,36) (Table III). However, another study using the same tool found no relationship between catastrophizing and non-adherence (34).
Of the 5 studies analyzed, the study measuring catastrophizing with The Catastrophizing Subscale (CSQ-CAT) (30) found that catastrophizing was associated with an increased risk of opioid misuse (r = 0.45, p < 0.001), although this result was not significant when evaluated alongside anxiety and depression.
DISCUSSION
The lack of adherence to analgesic treatment in patients with CNCP has been described above. However, studies analyzing psychological factors associated with analgesic adherence in these patients are scarce, and the results are inconsistent.
Among the results obtained in the review, depression is the variable that has been most studied in its association with analgesic adherence in patients with CNCP, being found in 8 out of the 14 articles included in this review that depression is a risk factor for low adherence. Similarly, the relationship between anxiety and adherence was analyzed in 6 studies, showing in two studies that its presence was associated with lack of adherence specifically with opioid treatment (30,35). In line with these results, Broekmans et al. (28) show a lack of adherence due to overuse when scores on the HADS scale are high, and Feingold et al. (27) show that anxiety is a higher risk factor for opioid misuse when it occurs concomitantly with depression. These results are relevant if we consider that anxiety and depression occur frequently in conjunction (38), and it has been described that there is a two-way relationship between both processes that could affect treatment adherence in patients with CP (39).
Moreover, the diversity of the results observed in the studies, which could be explained by the variety of methods used to evaluate depression and anxiety and the different way of measuring adherence, should be noted as a remarkable result. Timmerman et al. (11)highlighted these limitations in the various studies analyzed in their review, and they noted the difficulty that this causes in the interpretation of the results.
One fact frequently observed in the studies is the consideration of adherence as a dichotomous variable (adherence versus non-adherence), without delving in specific aspects included in this construct despite it has been shown that adherence follows a complex pattern of behavior that is difficult to evaluate from a binary response (40). Similarly, the differentiation between intentional or unintentional adherence suggested by other authors (41) was considered only in one of the studies included in the review (28), which constitutes an added limitation in the proper assessment of adherence.
The relationship between coping strategies and lack of adherence to treatment has been analyzed in 2 of the articles in this review, showing that while active coping strategies are related to lack of adherence due to lack of use, passive strategies are related to lack of adherence due to overuse. In a newly published meta-analysis, Hagger and Orbell (42) note that when patients perceive the disease as controllable, they use more active coping strategies, whereas when they perceive it as uncontrollable, the strategies used are more passive. These results could explain ours and give more credibility to the hypothesis that patients using more active coping strategies and thinking that they can cope with CP without treatment may believe they do not need to take the medication. By contrast, patients perceiving their disease as uncontrollable and using more passive coping strategies may think that the pain will be more bearable if they take medication.
The results on the relationship between catastrophizing and adherence shown in the review are inconsistent, even when the tool used to assess catastrophizing is the same. Different authors have reported that catastrophizing can negatively skew the perceptions and experiences of the patients, creating types of passive behaviors, such as rumination or impotence, and play an important role in the CP experience (43,44). It has been shown that patients who tend to experience pain with catastrophic vision are more vulnerable to the misuse of opioids because they may manifest unrealistic beliefs about pain and its consequences (45).
One fact also observed in our study is the lack of relationship between catastrophizing and misuse of opioids when this factor was evaluated together with anxiety and depression (33). This result could be explained because anxiety and depression are strongly related to catastrophizing, both processes being able to have a mediating role in the relationship between catastrophizing and the misuse of opioids, as Arteta et al. shows in their study (46).
The present study has some limitations, among which we noted the small number of articles meeting the inclusion criteria, which also only analyzed some psychological factors without considering other factors such as borderline personality disorder or neuroticism. It can also be a limitation that we did not specify all variables separately in the search strategy within the keywords instead of just the word “psychology”. However, we believe that this more generic strategy would provide us with global information and in line with the objective of the study.
Another limitation is that derived from the diversity of scales used and the different methods for measuring adherence that difficult the analysis of the results. It is also necessary to point out that adherence or lack of adherence is not always the responsibility of the patient, but may also be due to variables associated with care processing and communication, so this aspect must also be studied.
As a strength of the study, we would like to point out that the results obtained are from the search performed in 4 databases and that the topic is novel and shows the need to analyze other psychological factors that may be important in adherence to treatment in patients with CNCP.
CONCLUSIONS
Little attention has been paid in the scientific literature to the relationship between adherence to analgesic treatment and psychological factors in patients with CNCP, and inconclusive results have also been found in studies addressing the issue. Despite this, there is some agreement showing that the presence of depression and/or anxiety are associated with the lack of analgesic adherence observed in patients. However, other factors such as coping, catastrophizing, or other factors with potential effect on adherence need to be better studied.
ACKNOWLEDGMENTS
We would like to thank the Sistema Nacional de Garantía Juvenil and the Youth Employment Operational Program 2014-2020, with the European Social Fund (ESF), for the contract as technical support and management staff of the author’s R+D+i Jenifer Palomo-Osuna.
CONFLICTS OF INTEREST
The authors state that they have no conflicts of interest.
SOURCES OF FUNDING
The present study has not received specific funding from the public or the commercial sector agencies or non-profit organizations.
REFERENCES