DOI: 10.20986/resed.2020.3749/2019
ORIGINAL
Consumption of drugs used for the treatment of musculoskeletal pain in a cohort of manual workers in Zaragoza (Spain)
Consumo de fármacos utilizados en el tratamiento del dolor musculoesquelético en una cohorte de trabajadores manuales de Zaragoza (España)
E. Gaspar Calvo1
M. J. Lallana Álvarez2
S. Malo3,4
1Centro de Salud Las Fuentes Norte, Servicio Aragonés de Salud. Zaragoza, España
2Servicio de Farmacia de Atención Primaria Sector Zaragoza III, Servicio Aragonés de Salud. Zaragoza, España
3Departamento de Medicina Preventiva y Salud Pública. Universidad de Zaragoza. España
4Instituto de Investigación Sanitaria (IIS) de Aragón. Zaragoza, España
ABSTRACT
Introduction: The high prevalence of musculoskeletal diseases (MSDs) in certain populaion groups may cause a high consumption of non steroideal antiinflamatory drugs (NSAIDs). The present study aims to identify the continuous consumers of NSAIDs in a cohort of workers, who mainly perform manual tasks, analyzing the use of other drugs prescribed for the treatment of musculoskeletal pain (MSP).
Material and methods: Observational retrospective study. It has been analyzed data of all subjects, included on the AWHS (Aragon Workers Health Study) cohort, who received at least one NSAID prescription during 2016. It has been calculated the rate of use of NSAID, as well as the number of DDD per 1000 inhabitants per day (DHD). It has been identified continuous consumers, as those who used 182 defined daily dose (DDD) or more. For this group, it has been analyzed all prescriptions including other drugs used to treat MSP.
Results: The rate of use of NSAIDs in the AWHS cohort in 2016 was 41.6% (95% CI: 40.1%-42.7%), being higher in women (47.0%, 95% CI: 41.9%-52.1%). 5.7% of NSAID users were continuous consumers. Among them, etoricoxib was the most used NSAIDs (4,9 DHD), followed by ibuprofen (4,0 DHD). Refering to other drugs prescribed for MSP, the prescription rate of tramadol for continuous consumers was 24.2% (95% CI: 16.9%-23.3%) and benzodiazepines 3.0% (95% CI: 0.1%-6.0%).
Conclusions: NSAID consumption in the AWHS cohort appears to be higher than in general population. Continuous consumers preferably used NSAIDs with lower cardiovascular risk. The consumption rate of weak opioids was high for continuous users.
Key words: Non-steroidal anti-inflamatory drugs, analgesics, opioids, musculoskeletal diseases, chronic pain pharmacological therapy
RESUMEN
Introducción: La alta prevalencia de enfermedades musculoesqueléticas (EME) en determinados grupos de población puede condicionar que el consumo de antiinflamatorios no esteroideos (AINE) sea elevado. El presente estudio pretende identificar a los consumidores continuados de AINE en una cohorte de trabajadores que realizan fundamentalmente tareas de tipo manual, analizando el uso que hacen de otros fármacos indicados en el tratamiento del dolor musculoesquelético (DME).
Material y métodos: Estudio observacional retrospectivo, en el que se han analizado los datos, recogidos en la base de consumo farmacéutico Farmasalud, de todos los sujetos de la cohorte AWHS (Aragon Workers Health Study), que presentaron al menos una receta de un AINE durante el año 2016. Se ha calculado la tasa de utilización de AINE, así como el número de dosis diarias definidas (DDD) por 1000 habitantes por día (DHD). Se han identificado los consumidores continuados como aquellos que utilizaron 182 DDD o más. Para este grupo de consumo, se han analizado otros fármacos prescritos que suelen asociarse al tratamiento del DME.
Resultados: La tasa de utilización de AINE en la cohorte AWHS en 2016 fue del 41,6 % (IC 95 %: 40,1-42,7 %), siendo mayor en mujeres (47,0 %, IC 95 %: 41,9-52,1 %). El 5,7 % de los usuarios de AINE se consideraron consumidores continuados. Dentro de este grupo, el etoricoxib fue el AINE más utilizado (4,9 DHD), seguido de ibuprofeno (4,0 DHD). En cuanto a otros fármacos relacionados con el tratamiento del dolor musculoesquelético, la tasa de prescripción de tramadol en los consumidores continuados de AINE fue 24,2 % (IC 95 %: 16,9-23,3 %) y la de benzodiazepinas 3,0 % (IC 95 %: 0,1-6,0 %).
Conclusiones: El consumo de AINE en la cohorte AWHS fue más elevado que el reportado en la población general. Los consumidores continuados utilizaron preferentemente AINE con un menor riesgo cardiovascular. La tasa de consumo de opioides débiles, en los consumidores continuados de AINE, fue elevada.
Palabras clave: Antiinflamatorios no esteroideos, analgésicos opioides, enfermedades musculoesqueléticas, tratamiento farmacológico dolor crónico
Correspondence: Elena Gaspar Calvo
egaspar@salud.aragon.es
Received: 18-06-2019
Accepted: 23-03-2020
INTRODUCTION
Musculoskeletal diseases (MSDs) are frequently reported in the adult population (1), constituting one of the most frequent reasons for medical visits (2), as well as the leading cause of chronic pain (3). The 2017 National Health Survey includes osteoarthritis (OA) and chronic back pain, both cervical (15.8 %) and lumbar (19.8 %), among the most prevalent health problems in the Spanish population, OA affects 18.3 % of this population (1). In addition, almost half of the population reported having had pain in the last 4 weeks, which has interfered quite or much in daily life in 9.7% of cases (1). This is why the indication of analgesic treatment is generally high.
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) for the treatment of this type of ailments is widespread, both because of their high prescription and because they are easily accessible as self-medication. In those people with chronic MSDs, consumption is usually high, with an increased risk of gastrointestinal, renal or cardiovascular adverse effects due to the use of NSAIDs (4,5,6,7,8,9,10,11).
In a study based on the Finnish population, Helin-Salmivaara et al. found an increased risk of gastrointestinal bleeding 5.2 times (95% confidence interval [CI]: 4.7-5.9) more common among continuous consumers (≥ 182 DDD one year) of NSAIDs than in occasional consumers (12). Sánchez Serrano et al found, in a cohort study on the Spanish population, that ibuprofen and other propionic acid derivatives increase cardiovascular risk over time: Relative risk (95 % CI) 2.6 (2.2-3.1), increase after one month of consumption 1.0 (1.0-1.0), p < 0.001 (13). In another cohort study, Abajo et al found a significant increase in the risk of non-fatal acute myocardial infarction associated with long-term use (> 1 year) of NSAIDs (OR = 1.4; 1.1-1.8) (14).
Along with NSAIDs, other drugs are used in the management of chronic pain. Opioid (narcotic) and non-opioid analgesics, certain antidepressants, and benzodiazepines are frequently combined, following the recommendations of the pain ladder of the World Health Organization (WHO) for pain management, which was developed in 1986 (and updated in 1996) (15) to help control pain in cancer patients. Today, it is also used for the management of chronic pain, including pain caused by MSDs.
MSDs are the most common work-related health problem in Europe. According to the European Agency for Safety and Health at Work, almost 24% of workers in the European Union reported back pain and 22% reported muscle aches, being the neck, shoulders and upper limbs the most frequently affected areas (16). The present study has been performed a cohort consisting mainly of workers performing production work (17), which includes repetitive movements and long-term postures. In this context, a high prevalence of MSD is assumed, which would lead to high consumption of NSAIDs.
Thus, the objective of this study was to identify and characterize the different groups of NSAID consumption in a cohort of workers, with special attention to the continuous consumers, analyzing their use of other drugs indicated for the treatment of pain.
MATERIAL AND METHODS
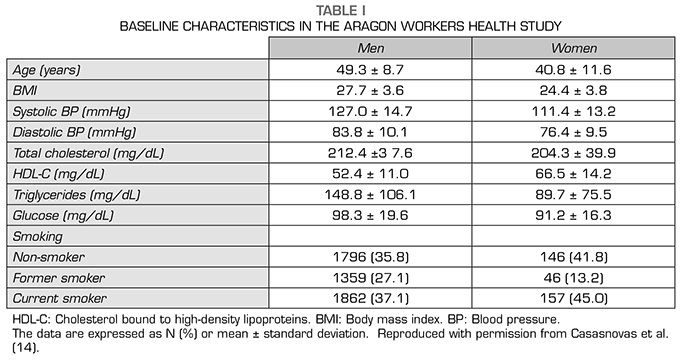
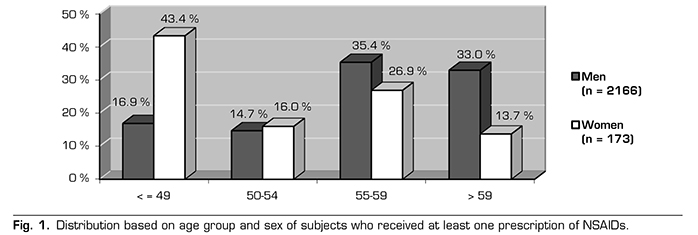
A retrospective observational study has been performed. The study population was composed by all the workers of THE OPEL ESPAÑA vehicle assembly plant in Figueruelas (Zaragoza, Spain), who during the years 2009-2010 agreed to participate in the Aragon Workers Health Study (AWHS). The AWHS is a cohort study designed to evaluate, through standardized clinical examinations, the trajectory of traditional and emerging cardiovascular risk factors. In addition, its association with the prevalence and progression of subclinical atherosclerosis in a population of middle-aged workers in Spain (17). The cohort consists of a total of 5650 individuals, of whom 92.2 % are men. Cohort follow-up continues today. Table 1 shows the baseline characteristics of AWHS.
For the present study, AWHS participants whose pharmaceutical benefit was covered by the Aragonese Health Service, who presented at least one prescription of an NSAID drug during the year 2016, were selected.
Information on the NSAIDs dispensed was obtained from the Pharmaceutical Consumption Information System of the Community of Aragon (FarmaSalud), which includes all drugs dispensed in the pharmacies of Aragon, prescribed by official medical prescription and charged to the Aragon Health Service. Drug identification was performed considering the ATC (acronym for Anatomical Therapeutic Chemical) classification system proposed by the WHO (18). This system allows each active substance to be identified by an alphanumeric code of seven elements according to the pharmacological group, the therapeutic subgroup, the chemical subgroups and the chemical substance.
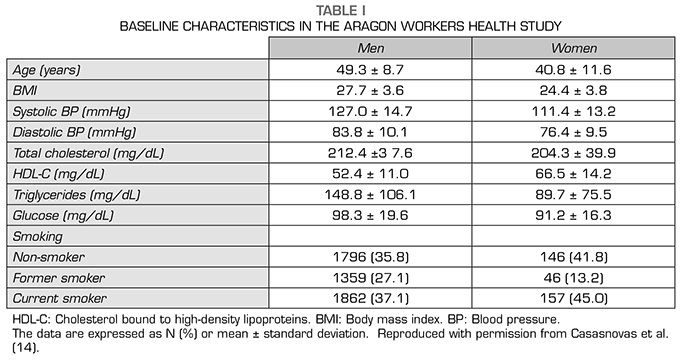
Annex 1 compiles the ATC codes and active principles of all NSAIDs used in 2016 in the AWHS cohort. The pharmacological subgroups belonging to group M01A (anti-inflammatory and nonsteroidal anti-rheumatic drugs) studied were: Acetic acid derivatives (M01AB), oxicams (M01AC), propionic acid and derivatives (M01AE), fenamates (M01AG) and coxibs (M01AH). The M01AX subgroup (other nonsteroidal anti-inflammatory and anti-rheumatic agents) has been excluded from the study, they cannot be considered as NSAIDs because of their composition and mechanism of action.
Consumption charged to mutual or other insurance companies was not included in the present study, nor was hospital consumption, private prescription consumption, or over-the-counter (basically self-medication) dispensing.
Data analysis
The descriptive analysis of the characteristics of the subjects included in the present study, as well as of the dispensed prescriptions, were performed.
The rates of patients treated with NSAIDs, by sex and by age group, were calculated separately and together to measure NSAID use. The results have been expressed per hundred subjects. The confidence level (CI) set for the calculation of rates was 95 %. The exact method has been used to calculate the 95% CI of the rates in population groups of less than 30 subjects, whereas for groups with a number of 30 or more individuals the approximate method has been used.
To explore the use of NSAIDs in the group of workers and to classify them by consumer groups, the criterion defined by Helin-Salmivaara et al. (12) was used. This criterion considered as continuous consumers those who used at least 182 defined daily doses (DDD) in one year; consumers between 31 and 181 DDD were classified as moderate consumers. Whereas those with a consumption of less than or equal to 30 DDD formed the occasional consumer group (12). DDD are technical units of measurement defined by WHO as the mean dose, per day, for a drug used for primary indication, in adults (18).
The distribution by sex in the three consumption groups was studied, as was the association between the two variables using the Chi-square test. The age differences between the different consumption groups were analyzed using the non-parametric Kruskal-Wallis test.
The pattern of NSAID consumption has been determined by calculating the number of DDD per 1000 inhabitants per day (DHD) of the 10 most commonly used active ingredients for each consumption group.
Finally, the use of other drugs generally used in the treatment of MSP, such as analgesics (N02), has been studied in continuous consumers. Within the opioid subgroup (N02A), fentanyl (N02AB) and tramadol (N02AX) have been analyzed. For other analgesics (N02B), acetaminophen (paracetamol) (N02BE01) and metamizole (N02BB02) have been assessed. The prescriptions for antidepressants (N06AB) and anxiolytics derived from benzodiazepine (N05BA), namely diazepam (N05BA01) and ketazolam (N05BA10), which can be used as muscle relaxants according to their data sheet, were also reviewed.
Ethical aspects and conflict of interest
Subjects who agreed to participate in the AWHS signed an informed consent form (17). All data were received and used in an anonymized manner, and it was impossible to identify the studied subjects. Finally, this study has been approved by the Ethical Committee of Clinical Research of Aragon (CEICA).
The present study has not received specific funding from public sector entities, the commercial sector or non-profit organizations.
The authors declare that they have no conflict of interest.
RESULTS
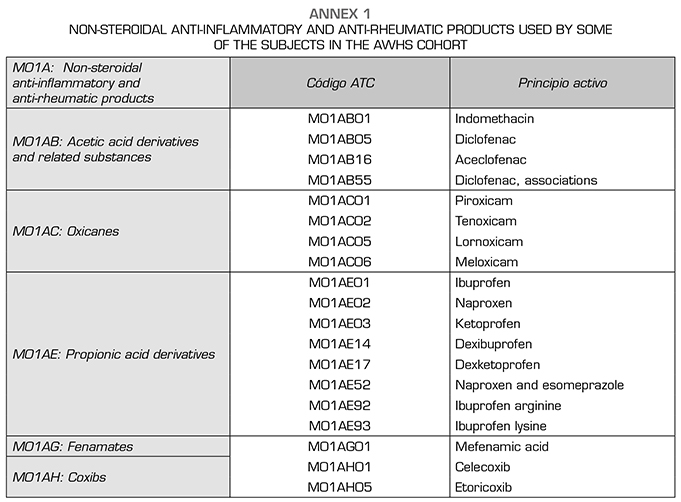
The total number of subjects who received at least one NSAID prescription in 2016 was 2339, of whom 92.6 % were men. A total of 21.3 % of subjects received this prescription during the first trimester of 2016. The median age of the treated subjects was 57 years (interquartile range [IR] = 52-60). Figure 1 represents the distribution of subjects by age and sex groups.
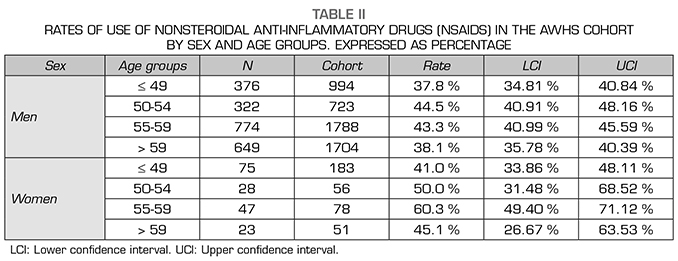
The rate of NSAID use in the AWHS cohort was 41.6% in 2016 (95% CI: 40.1 %-42.7%), being higher in women (47.0%, 95% CI: 41.9-52.1%) than in men (41.6%, 95% CI: 40.2-42.9 %), although the differences were not significant.
The results were similar among the different age groups, in both men and women (Table 2). For all age groups, rates were higher in women, although differences were not statistically significant.
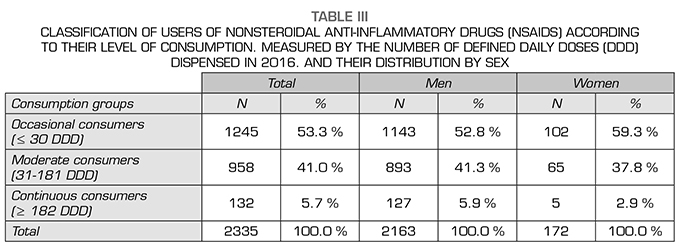
A total of 53.3 % of NSAID users were classified as occasional consumers, i.e. they had an annual consumption of less than or equal to 30 DDD. Whereas 41 % were classified as moderate consumers (between 31 and 181 DDD), and 5.7 % were considered continuous consumers, with a total annual DDD of more than 181 (Table 3).
A total of 52.8 % of men had occasional consumption compared with 5.9 % who were considered conti-nuous consumers. In the case of women, 59.3 % had occasional consumption compared to 2.9 % of continuous consumption. The association between sex and the consumption group was not significant (p = 0.1).
The study of age by consumption groups showed statistically significant differences between the 3 established groups (p < 0.001). In subjects with occasional consumption, the median was 56 years (RI = 50-60), among moderate consumers the median age was 58 years (RI = 47-61), while in continuous consumers the median age was 59 years (RI = 56-63).
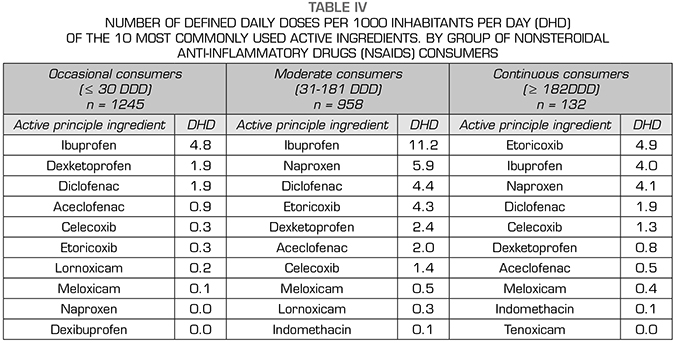
The use of NSAIDs, measured in DHD, in the different consumption groups is shown in Table 4, which reflects the 10 most used active ingredient in each group. Occasional consumers preferentially used ibuprofen (4.8 DHD), followed by dexketoprofen and diclofenac, 1.9 DHD each. Moderate consumers mainly used ibuprofen, with 11.2 DHD. In the continuous consumer group, etoricoxib was the most widely used NSAID (4.9 DHD), followed by ibuprofen (4.0 DHD).
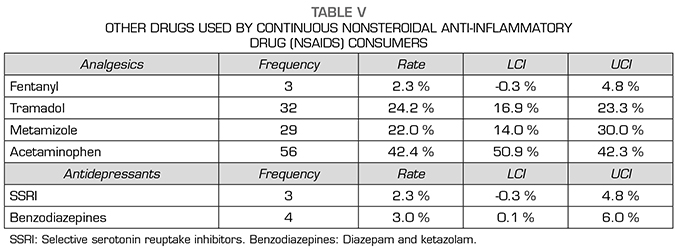
The descriptive analysis of other drugs used by the group of continuous NSAID users is shown in Table V. With regard to the pharmacological treatment of MSP, within the analgesic group the use of acetaminophen is highlighted, its rate was 42.4 % (95 % CI: 50.9-42.3 %). The use of tramadol was 24.2 % (CI 95 %: 16.9-23.3 %), whereas the rate of benzodiazepine use among continuous NSAID users was 3.0 % (95 % CI: 0.1-6.0 %).
DISCUSSION
Nearly half of the subjects in the AWHS cohort received at least one NSAID prescription in 2016 and the utilization rate was higher in women. Continuous consumers account for about 6% of all NSAID users and their median age was higher than that of moderate and occasional consumers. In addition to NSAIDs, continuous consumers used acetaminophen, tramadol, diazepam and ketazolam.
Other studies have reflected the rate of use of NSAIDs in the general population (19). A study conducted in Navarre reveals that 14.0 % of the population was treated with an NSAID at some point during the first three months of 2016, a rate of 7 points lower than that found in the AWHS cohort for the same period. This difference may be due to the high median age in the subgroup of the studied cohort. The prevalence of MSDs increases with age, so it seems reasonable that NSAID consumption is higher in the cohort than in the general population. Furthermore, should be taken into account the fact that the individuals studied are mostly manual workers (17). The 2015 National Survey of Working Conditions states that 84% of workers surveyed report that they are “always or almost always” or “often” exposed to some poor aspect of the physical demands of their jobs. The most common physical demands are the repetition of the same movements of the hands or arms (69.0 %) and the adoption of painful or fatiguing postures (54.0 %) (20). Therefore, the incidence of MSD in the AWHS cohort could be higher than in the general population, which would justify the high rate of use of NSAIDs.
According to the 2008-2009 Women and Health Report in Spain, women are 1.8 times more likely to have a chronic problem and 1.5 times more likely to be limited in their activity because of that problem, compared to men, regardless of age, social class, the cultural level or the working situation. In relation to MSDs in women, OA is seen to increase with age and is more frequent between the ages of 45 and 64. Back pains (cervical and lumbar) also increase with age, but they reach high prevalence already in the group of 30 to 44 years (21). All of this could justify a higher consumption of NSAIDs in females. In our study, a higher rate of NSAID use has been found in women than men, but the differences have not been significant. This is attributable to the fact that the number of women in the AWHS cohort, as well as among NSAID users, is low.
The use of NSAIDs by consumption group in the AWHS cohort does not follow the standard of prescription by active principle in the Spanish population in 2016: Ibuprofen, naproxen, etoricoxib (2). It is surprising that etoricoxib has been the most prescribed active ingredients among continuous consumers/users, ahead of ibuprofen and naproxen, although the latter are considered safer for the cardiovascular system (22). Among the continuous consumers, the consumption of etoricoxib was significantly higher (4.9 DHD) than that of the Spanish population in 2016 (3.6 DHD).
Regarding other drugs used by continuous NSAID users, we note that almost half received acetaminophen in 2016. Acetaminophen is one of the most widely used drugs to treat pain due to its efficacy and high safety profile. However, a review of recent data points to the gastrointestinal and cardiovascular toxicity of acetaminophen and to its low analgesia capacity in OA (23). This has led Osteoarthritis Research Society International (OARSI) to modify its recommendation regarding the use of this drug in patients with comorbidities as “uncertain” (24). Therefore, it would be advisable to review and detect, among the subjects in the cohort, those cases in which the prescription of acetaminophen is not advisable.
In the present study, a high tramadol utilization rate was found among the continuous NSAID users in the cohort. This finding would be in line with the report of the Catalan Health Service on the risks associated with the concomitant use of opioids and benzodiazepines, which indicates that in 2016, 6.4 % of the Catalan population received one or more prescriptions for an opioid drug, of which 25 % used tramadol (73,3 %) (25). In the same way, various voices in our country warn that consumption of these potent analgesics has soared in recent years (25,26). The report on the use of opioid drugs in Spain prepared by the Spanish Agency for Medicinal Products and Health Products (AEMPS) reflects the increase in tramadol consumption, from 1.8 DHD in 2008 to 5.3 DHD in 2015 (27). In contrast, a population-based Portuguese study analyzing the use of various pain relief drugs in patients with chronic active low back pain found a very low opioid utilization level (1.6%), even for those with severe pain (28). The fact that the collection of information was conducted through a personal interview and not by using pharmaceutical dispensing databases may have influenced the attainment of such low rates. The negative effects of opioids, including tramadol, on the central nervous system and the risk of abuse and addiction, if used for more than six months, should be recalled (26). Therefore, these drugs are considered a second-line treatment for the management of chronic non-oncological pain and, as recommended by clinical practice guidelines, their use should be considered only when the expected benefits in pain and function are higher than the patient’s risk (Category A recommendation; type 3 evidence) (29).
Another drug used by continuous consumers, in relation to the treatment of chronic pain due to the muscle relaxation effect, was benzodiazepines. Population-based studies collect the prescription rate of these drugs in different countries, showing a wide variability. In Ireland, the rate for persons over 16 years of age was 16.6 % (95 %: CI 16.5-16.7 %) in 2015 (30). In a study in Switzerland, 9.1% of adults surveyed (n = 45309) had received at least one prescription within a 6-month period (31). In the United States, the Medical Expenditure Panel Survey (MEPS), conducted in 2013, indicated that 5.6% of adults over the age of 18 had received at least one prescription of benzodiazepine (32). However, no studies have been found that explicitly quantify the use of benzodiazepines as muscle relaxants. Moreover, the prevalence of anxiety disorders in Spain is 6.2%, according to the European Study on the Epidemiology of Mental Disorders (ESEMeD-Spain) (33). The result found in our study could lead us to think of a low use of these drugs for the treatment of MSD. However, the analyzed database does not collect information on the diagnosis associated with the prescription, so the therapeutic indication of the prescription could not be verified.
Limitations and Strengths
As limitations of the study, it should be noted that DDD is a technical unit of measurement and does not necessarily reflect the actual daily dose prescribed or used by the patient, although it should be close to it. Furthermore, the data handled do not allow to know the compliance of the treatments; therefore, the terms utilization (or consumption) should not be interpreted in a literal sense. In any case, this is a “real-life” study, which provides information on the usual therapeutic practice.
Self-medication and hospital and private consumption remain excluded from this study. However, it is assumed that over the counter (OTC) consumption may be high, because it has been previously reported by other studies. In Norway, a large population survey found that the prevalence of OTC NSAID use was 19.0% (34). Another survey in 2009 in Australia found that 26.0 % had used an OTC NSAID, mainly ibuprofen (99.0 %) (35). In Spain, the National Health Survey indicates that 10.1% of the population self-medicated in 2016 and 29.9% of the drugs used were drugs for pain relief (36).
For the present study, no data were available on the existence of previous MSDs or other comorbidities that could have influenced NSAID consumption in the cohort analyzed.
The characteristics of the cohort, with a low presence of women and a very limited age range, make the studied population not representative of the general population. However, the study of an active population is relevant, since it is less demanding of health care than other population groups (children and the elderly, for example) and is not usually the subject of specific health interventions.
As strengths, we emphasize that the database analyzed in the present study, Farmasalud has been used in other previous studies (37,38,39,40), constituting a valid tool and with good record quality. We would like to emphasize that there are no recent studies in Spain on the use of NSAIDs and other drugs related to the treatment of MSDs.
CONCLUSIONS
In conclusion, this study shows the high use of NSAIDs in a cohort of mainly manual workers. In addition, continuous consumers preferred NSAIDs with lower cardiovascular risk, such as etoricoxib or ibuprofen. Furthermore, data is provided on their use of other drugs used in the management of chronic pain caused by MSDs, such as acetaminophen, tramadol and benzodiazepines, are provided.
Based on the results obtained, further research could be developed focusing on groups of populations with high prevalence of MSD, such as people over 65 years or women, which would allow to associate prescription with medical diagnosis, with the aim of determining the magnitude of NSAID consumption, whose use is associated with an increased cardiovascular, digestive, and renal risk, as well as with the use of other drugs, such as opioids, because of the known risk of abuse that exists.
REFERENCES