doi.org/10.20986/resed.2022.4039/2022
ORIGINAL
THE IMPACT OF BUPIVACAINE DOSE ON POST SPINAL SHIVERING IN CESAREAN SECTION: A RANDOMIZED TRIAL
EL IMPACTO DE LA DOSIS DE BUPIVACAÍNA EN EL ESCALOFRÍO POSTESPINAL EN LA CESÁREA: UN ENSAYO ALEATORIZADO
A. S. Wesam-Eldin1
S. I. Ezzeldin1
A. E. Abd-Elazeem1
1Department of Anesthesia and intensive care. Faculty of Medicine. Menoufia University, Menoufia, Egypt
ABSTRACT
Objective: The aim of this study was to investigate the relationship between the intrathecal dose of hyperbaric bupivacaine and the incidence and severity of post spinal shivering in parturients undergoing cesarean section.
Material and methods: A hundred full term pregnant ladies undergoing elective cesarian section were randomized into two equal groups according to bupivacaine dose given for spinal anesthesia. low dose bupivacaine group (LB group) and high dose bupivacaine group (HB group) received 8 mg and 10mg bupivacaine respectively. The incidence and severity of shivering were recorded as primary outcomes. Other measurements were heart rate, mean arterial blood pressure, tympanic membrane temperature, sensory block level.
Results: The level of spinal block was higher in HB group compared with LB group (p = 0.02). The incidence of intra-operative shivering was 15 (30 %) in HB group and 10 (20 %) in LB group (p = 0.032) while the shivering scores were not significant. The incidence of postoperative shivering was 16 (32 %) in HB group and 11 (22 %) in LB group (p = 0.043). Intra-operative tympanic membrane temperatures showed a highly significant reduction from the baseline (p < 0.0001) while postoperative values showed no significant difference from the baseline.
Conclusions: The level of the spinal block rather than the dose of intrathecal bupivacaine affects the incidence of shivering. At low levels of the spinal block the incidence of shivering is decreased with no effect on the degree of shivering.
Key words: Spinal anesthesia, bupivaciane, shivering, cesarian section
RESUMEN
Objetivo: El objetivo de este estudio fue investigar la relación entre la dosis intratecal de bupivacaína hiperbárica y la incidencia y severidad de los escalofríos postespinales en parturientas sometidas a cesárea.
Material y métodos: Cien mujeres embarazadas a término que se sometieron a una cesárea electiva se distribuyeron aleatoriamente en dos grupos iguales de acuerdo con la dosis de bupivacaína administrada para la anestesia espinal. El grupo de bupivacaína de dosis baja (grupo LB) y el grupo de bupivacaína de dosis alta (grupo HB) recibieron 8 mg y 10 mg de bupivacaína respectivamente. La incidencia y la gravedad de los escalofríos se registraron como resultados primarios. Otras mediciones fueron la frecuencia cardiaca, la presión arterial media, la temperatura de la membrana timpánica y el nivel de bloqueo sensorial.
Resultados: El nivel de bloqueo espinal fue mayor en el grupo HB en comparación con el grupo LB (p = 0,02). La incidencia de escalofríos intraoperatorios fue de 15 (30 %) en el grupo HB y de 10 (20 %) en el grupo LB (p = 0,032), mientras que las puntuaciones de escalofríos no fueron significativas. La incidencia de escalofríos postoperatorios fue de 16 (32 %) en el grupo HB y de 11 (22 %) en el grupo LB (p = 0,043). Las temperaturas intraoperatorias de la membrana timpánica mostraron una reducción muy significativa con respecto a la línea de base (p < 0,0001), mientras que los valores postoperatorios no mostraron diferencias significativas con respecto a la línea de base.
Conclusiones: El nivel de bloqueo espinal más que la dosis de bupivacaína intratecal afecta la incidencia de escalofríos. A niveles bajos de bloqueo espinal, la incidencia de escalofríos disminuye sin efecto sobre el grado de escalofríos.
Palabras clave: Anestesia espinal, bupivacaína, escalofríos, cesárea
Recibido: 06-11-2022
Aceptado: 20-12-2022
Correspondence: Sultan Wesam-Eldin
wesamsultan@med.menofia.edu.eg
INTRODUCTION
Shivering is a common undesirable event after spinal anesthesia in parturients undergoing cesarean section (1,2). Spinal anesthesia impairs the central thermoregulatory mechanism and redistributes blood between body compartments (2,3). Hypothermia is common in association with neuraxial block due to the redistribution of blood between the different body compartments and impaired central thermoregulatory control (4). Intravenous fluids and cold operating rooms are other contributing factors. Hypothermia has its negative effects on patients such as delayed recovery from anaesthetics, increased cardiac events, and postoperative shivering (3,5). Although shivering is a protective mechanism by increasing heat production, but it is associated with side effects such as increased oxygen consumption, patient discomfort, and monitoring interference (6). Few drugs have been used intrathecally or intravenously to prevent and treat post spinal shivering. Many studies investigated the use of different drugs (meperidine, ketamine, midazolam, sufentanil, nalbuphine, ondansetron, clonidine, or tramadol) for prophylaxis and treatment of post spinal shivering (7,8,9). In our literature review we did not find a study to show the impact of the dose of intrathecal hyperbaric bupivacaine or the level of the neuraxial block on the incidence and severity of post spinal shivering. We hypothesized that the level of spinal anesthesia can affect the severity of post spinal shivering. The aim of this study was to show the relationship between the intrathecal dose of hyperbaric bupivacaine and the incidence and severity of post spinal shivering in patients undergoing cesarean section in a prospective double blinded randomised trial.
MATERIAL AND METHODS
Trial design and participants
Ethical approval for this study (MenoufiaU2015/2) was provided by the Ethical Committee Menoufia University Hospitals (Chairperson Prof Mohamed Kandeel) through approval of the department of anesthesia and intensive care Ethics Committee for Clinical Research, Menoufia, Egypt, (Chairperson of Ethics Committee of anesthesia and intensive care department Prof Hatim A. Ataalah) at January 21, 2015. The study was conducted at El Menoufia University hospital in the period between December 30, 2017 to September 29, 2018. Written informed consents were obtained from all patients. The included patients in the study were full term pregnant ladies scheduled for elective cesarean section, ASA I or II physical status, aged 22 to 35 years, with height of 150 cm to 170 cm and with no contraindication to spinal anesthesia. The excluded patients from the study were with contraindications to spinal anesthesia, high risk pregnancy, height < 150 cm or > 170 cm, baseline core body temperature ? 37.5 °C or ? 36.5 °C, acute fetal distress, and history of any metabolic disorder.
Randomisation
The patients were randomly assigned, according to bupivacaine dose given, into low bupivacaine (LB group) or high bupivacaine (HB group). One investigator generated the randomization sequence and provided allocation concealment by using sequentially numbered, sealed, opaque envelopes. Randomization was performed in balanced blocks with a 1:1 allocation ratio by a computer software (Random Allocation SoftwareVersion 1.0, May 2004. Developed by M. Saghaei, MD., Department of Anesthesia, Isfahan University of Medical Sciences, Isfahan, Iran. Email: msaghaei@yahoo.com).
Technique
10 ml kg-1 h-1 lactated Ringer’s solution was administered to all patients through an 18gauge intravenous (i.v.) cannula for 30 minutes as a preload before spinal anesthesia. The infusion rates were then reduced to 6 ml kg-1h-1. Intravenous and irrigation fluids were warmed to 37 °C with no further warming applied. The operative room temperature was adjusted at 21 to 24 ?C with humidity of 20-60 %. The patients’ lower limbs and arms were wrapped by one layer of cotton. Spinal anesthesia was performed under complete aseptic technique in the setting position (at L3-L4 or L4-L5 space) using 27 gauge pencil tipped spinal needle after 2 % lidocaine infiltration of the skin. In LB group, the patients were administered hyperbaric bupivacaine 0.5 %. 8 mg (1.6 ml) with added 25 µg fentanyl (0.5 ml) to form a total volume of 2.1 ml. In HB group, the patients were administered 10 mg hyperbaric bupivacaine 0.5 % (2 ml) with added 25 µg fentanyl (0.5 ml) to form a total volume of 2.5 ml. If the sensory block had not reached T8, or there was moderate pain during the skin incision, spinal anesthesia considered to be failed and the patient was withdrawn from the study. Phenylephrine infusion (50 µg ml-1) was attached to the infusion set via a non return valve. Using a syringe pump, phenylephrine infusion 60 ml h-1 was started immediately following the intrathecal injection. Hypotension was considered if the mean arterial blood pressure decreased greater than 20 % below baseline. A rescue bolus dose of 20 µg phenylephrine was given if hypotension occurred despite phenylephrine infusion and the total dose of phenylephrine used was recorded. Bradycardia was considered if the heart rate was less than 60 beats/min and was managed by i.v. 10-20 µg kg-1 atropine boluses. Intra-operative measures of warming i.v. fluids, control of room temperature and patient insulation were applied during patient follow up in the post anesthesia care unit.
Measurements
Shivering scores and the incidence of shivering were recorded as primary outcomes while other measurements were recorded as secondary outcomes.
The degree of shivering was assessed by the following scale: 0 = no shivering; 1 = piloerection but no visible muscle activity; 2 = muscular activity in one muscle group; 3 = muscular activity in more than one muscle group but not generalized movement; 4 = shivering involving the movement of the whole body (10). Shivering ( incidence and degree) was recorded in the intra-operative and postoperative period until complete recovery from the effect of the spinal anesthesia. i.v. nalbuphine 0.07 mg/kg was given if shivering score was ≥ 3 to be repeated until shivering was fully controlled and the total dose was recorded.
Before spinal anesthesia, the tympanic membrane temperature was recorded as a baseline and then every 10 minutes after spinal anesthesia till the end of surgery and postoperatively every 20 minutes till complete recovery from spinal anesthesia. Hypothermia was recorded as a core body temperature below 36 °C and was managed using warming blanket and warming i.v. fluids up to 42 °C.
Sensory block level was assessed by loss of cold sensation. Motor block was assessed by modified Bromage scale as follows: Grade 0 = No motor block; Grade 1 = Impaired hip flexion, normal knee and ankle movements; Grade 2 = Impaired hip and knee movements, normal ankle movement; Grade 3 = Impaired movements at hip, knee and ankle joints (11).
Vital signs including heart rate, mean arterial blood pressure, and peripheral oxygen saturation were recorded before spinal anesthesia as a baseline then every 10 minutes intra-operatively until the end of surgery and postoperatively every 20 minutes till complete recovery from spinal anesthesia.
Blindness of observer
A sterile independent anesthetist blind to the randomization and allocation of the study groups, was instructed to prepare the intrathecal study drugs and performed the spinal anesthesia. Another anesthetist, who was blinded to the dose and volume of the used drugs, observed the patient and collected the research data.
Power analysis
The sample size was calculated using GraphPad Instat statistics version 3. We conducted a pilot study and accordingly, the incidence of shivering was decreased by 24 % in the low bupivacaine group so that, the calculated sample size was total of 91 patients, with a level of significance 0.05 and power 90 %. In the current study, 100 patients were randomized to ensure reliable results.
Statistical analysis
Statistical analysis was done using SPSS 19 (SPSS Inc, an IBM company, Chicago, USA). The incidence of shivering and side effects were analyzed by the chi square test (χ2 test). Student t test was used for analysis of the vital signs and tympanic membrane temperatures. P < 0.05 was considered statistically significant.
RESULTS
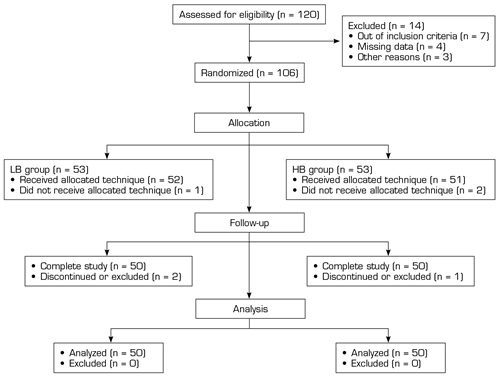
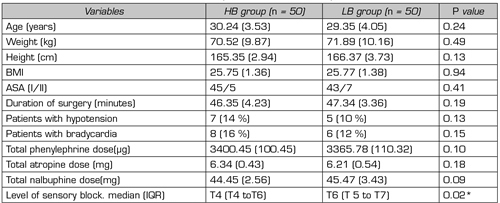
Figure 1 represents a flow chart of the study participants with a total number of 120 parturients recruited for the study but finally 100 parturients completed the study and analysis. The demographic data and peri-operative characteristics are represented in Table I. Hypothermia was observed intra-operatively in 20 patients (40 %) in HB group and 12 patients (24 %) in LB group (p = 0.013) while postoperative hypothermia was recorded in 17 patients (34 %) patients in HB group and in 13 patients (26 %) in LB group (p = 0.042). The incidence of intra-operative shivering was significantly higher in HB group 15 (30 %) compared with LB group 10 (20 %); (p = 0.032); The incidence of postoperative shivering was significantly higher in HB group 16 (32 %) compared with LB group 11 (22 %); (p = 0.043). Intra-operative and postoperative shivering scores were insignificant (p > 0.05); (Table II). Intra-operative tympanic membrane temperatures were not different between groups; p (95 % confidence interval CI) were 0.58 (-0.06 to 0.12), 0.42 (-0.07 to 0.17), 0.39 (-0.07 to 0.19), 0.57 (-0.12 to 0.22), 0.29 (-0.14 to 0.04) at 10, 20, 30, 40, 50 minutes respectively); however, they showed a highly significant reduction from the baseline (p < 0.0001); (Figure 2). Postoperative tympanic membrane temperatures were insignificant between groups; p (95 % CI) were 0.13 (-0.39 to 0.05), 0.58 (-0.13 to 0.23), 0.56 (-0.26 to 0.14), 0.49 (-0.11 to 0.23), 0.41 (-0.1 to 0.24) at 20,40,60,80,100 minutes respectively) and in each group compared with the baseline value (Figure 3). The intra-operative and postoperative vital signs (heart rate, mean arterial blood pressure, and oxygen saturation) showed no significant difference between groups. In each group, the intra-operative mean arterial blood pressure showed a highly significant reduction from the baseline (p < 0.0001) while the postoperative values showed no significant change from the baseline (p > 0.05) (Figures 4 and 5).
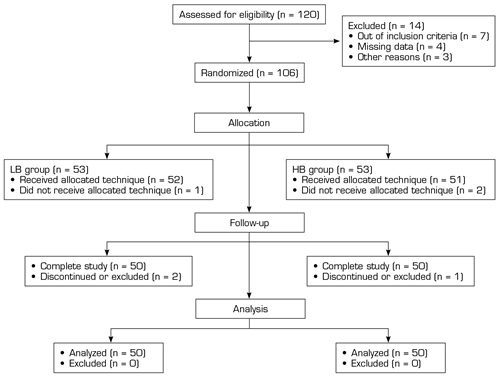
Fig. 1. Flow chart.
Table I.
Demographic data and peri-operative characteristics in HB (high bupivacaine group) and LB (low bupivacaine group). Data expressed as mean (SD), number, number (%) or median (interquartile range).
*Statistical significance. Statistical analysis by student t-test or X2.
Table II. Intra-operative and postoperative shivering scores in HB (high bupivacaine group) and LB (low bupivacaine group). Data expressed as number (%).
*Statistical significance (p < 0.05). Data analyzed by X2 test.
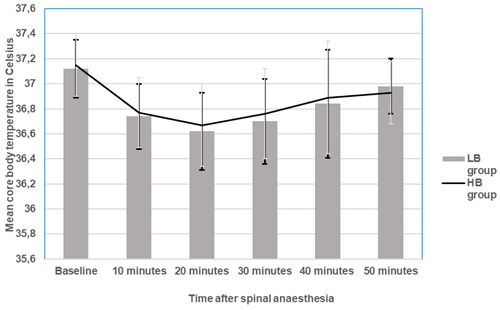
Fig. 2. Intra-operative core body temperature changes in HB (high bupivacaine group) and LB (low bupivacaine group). Data expressed as mean (SD). There is a highly significant reduction in both groups compared with the baseline value. No significant difference between groups.
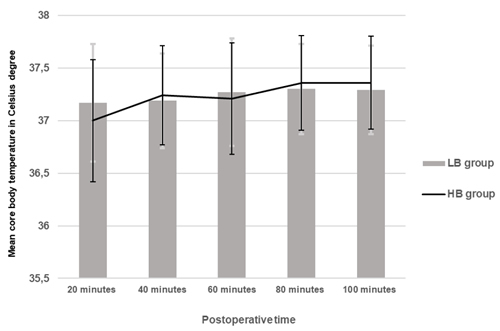
Fig. 3. Postoperative core body temperature changes in HB (high bupivacaine group) and LB (low bupivacaine group). Data expressed as mean (SD). No significant difference from the baseline or between the groups.
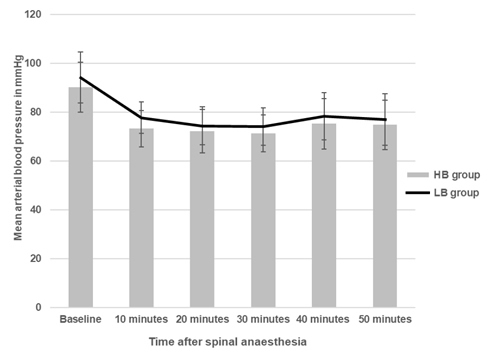
Fig. 4. Intra-operative mean arterial blood pressure changes in HB (high bupivacaine group) and LB (low bupivacaine group). Data expressed as mean (SD). There is a highly significant reduction in both groups compared with the baseline value. No significant difference between groups.
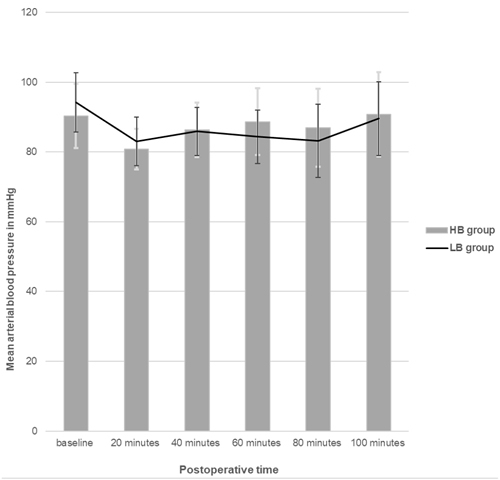
Fig. 5. Postoperative mean arterial blood pressure changes in HB (high bupivacaine group) and LB (low bupivacaine group). Data expressed as mean (SD). No significant difference from the baseline or between the groups.
DISCUSSION
Despite the availability of many drugs and a lot of anesthesia techniques shivering is a common observation seen in patients received general or regional anesthesia. The incidence of shivering can reach up to 62 % in parturients undergoing cesarian section under spinal anesthesia (1). The current study was designed to investigate the effect of two different doses of hyperbaric bupivacaine on the incidence of post spinal shivering in parturients undergoing elective cesarian section. The current study revealed a significant increase in the incidence of shivering in patients administered a high dose of intrathecal bupivacaine where the level of the spinal block was significantly high with no difference in the degree of shivering related to intrathecal bupivacaine dose or the level of the spinal block.
Sultan P and his colleagues conducted a study to determine the most appropriate method to reduce the incidence of shivering during cesarean section. Their study revealed that active warming by warm blanket and fluids reduced peri-operative hypothermia and shivering (12). In the current study, measures to maintain the patient’s body temperature constant were applied in the form of ambient temperature control, proper patient covering and using fluids at the patient’s body temperature. To uncover the impact of the level of the spinal block on shivering, active warming was only applied if hypothermia occurred.
Hypothermia after the neuraxial anesthesia was reported to occur due to three cofactors; the first one is heat redistribution between the core and peripheral tissues (13). The second cofactor is the heat loss to the environment. Neuraxial anesthesia leads to peripheral vasodilatation due to sympathectomy (14). This peripheral vasodilatation increases the heat loss to the environment and enhances the redistribution between the core and peripheral tissues. Other contributing factors are related to the spinal anesthesia which impairs the shivering response by muscle paralysis below the block and interferes with the sensory inputs below the level of the block leading to the inability of the patient to complain of coldness (15). The third cofactor of hypothermia is the altered central thermoregulatory response (16). This effect of spinal anesthesia on the thermoregulation was evaluated by Kurz and his colleagues who revealed that there is a correlation between extensive levels of block during spinal anesthesia and the low core temperature consistent with the known physiologic effects of spinal anesthesia. These effects were apparent below the level of the block so that the higher the block level, the more impairment of the thermoregulatory function is to be expected. They concluded that during spinal anesthesia, there is a reduction in the shivering and vasoconstriction thresholds consistent with thermoregulatory impairment due to altered afferent thermal inputs as a result of the block (17). The results of the current study were consistent with the observations of Kurz study where the incidence of hypothermia was increased in the HB group despite the strict measures in the study protocol to guard against hypothermia reflecting the great impact of the higher level of the block on the thermoregulatory response which was continued in the postoperative period.
Leslie K and his colleagues conducted a study on old men undergoing urological surgery to investigate the shivering threshold in relation to the spinal blockade level. The investigators revealed that core temperature threshold was decreased by 0.06 °C for each dermatomal level blocked. The authors concluded that at higher levels of spinal anesthesia the central thermoregulatory mechanisms were impaired more than at lower levels (18). Unfortunately, the authors used a technique that may compromise the safety of their patients because they administered i.v. ice-cold Ringer’s lactate solution before spinal anesthesia. It is unclear why the authors infused the ice-cold Ringer’s lactate to the patients and if this cold fluid can affect the thermoregulatory mechanism and body temperature. In contrast, the current study was conducted on pregnant ladies who commonly show a higher incidence of post spinal shivering and a different technique was used ensuring no compromise of the patients’ safety where factors contributing to hypothermia were almost controlled by keeping constant operating room temperature, warming all used fluids to the body temperature and proper insulation of the patients.
According to Leslie K and Kurz studies, the increased incidence of shivering in the HB group may be related to the high level of the spinal block rather than to the dose of bupivacaine administered. However, the degree of shivering was not affected by the dose of bupivacaine or the level of the spinal block which lacks explanation and may encourage further research.
Reports of the previous studies revealed that the use of low dose spinal anesthesia can reduce the incidence and severity of hypotension and its detrimental consequences (18,19,20,21,22,23,24,25).
Roofthooft and his colleagues conducted a review to evaluate the evidence of the use of low dose spinal anesthesia for the prevention of hypotension during cesarean section. They concluded that bupivacaine in a dose between 5 to 7 mg is enough for cesarean section to produce effective anesthesia with no serious impact on the maternal haemodynamics or the foetal outcome (26).
In contrast to these previous studies, the current study revealed no difference between high and low dose spinal anesthesia on the incidence of hypotension. This may be attributed to the use of continuous phenylephrine infusion and the fluid preloading which maintained a relatively stable blood pressure despite the reduction of the blood pressure from the baseline after spinal anesthesia.
A limitation to the present study was that the patient’s heights were not taken into consideration in calculating the dose of the intrathecal bupivacaine. To avoid a too high or low spinal block level, the range of the height limit of the patients included was determined between 150 cm and 170 cm.
Another limitation was the inability to observe shivering in the lower extremities during spinal anesthesia. To overcome this problem, grade 4 of the shivering score was considered when shivering involves simultaneously all the muscles of the upper half of the body.
In conclusion, the level of the spinal block rather than the dose of intrathecal bupivacaine affects the incidence of shivering. At low levels of the spinal block the incidence of shivering is decreased with no effect on the degree of shivering.
ACKNOWLEDGEMENTS
All the authors would like to thank the parturients who accepted to participate in this study.
REFERENCES